The humans the algorithms can't reach

For years, pharma has been racing toward a digital future built on chatbots, refill apps, automated workflows, and AI promising to finally solve adherence. It was sleek. It was logical. It felt inevitable. But here’s the shock: after all the innovation, the most important metric in the entire medication journey hasn’t moved at all.
Despite billions spent and decades of interventions, global adherence rates remain stuck at roughly 50%, almost exactly where the WHO first reported them more than twenty years ago.
Our team recently analysed a sample of more than 140,000 patient conversations, focused on four diverse disease states: diabetes, chronic kidney disease (CKD), cardiovascular disease, and migraine. Each was chosen for their range in treatment complexity, symptom visibility, and patient experience. While technology has improved everything around the medication journey – faster workflows, smarter notifications, and more intuitive portals – the emotional experience at its core has been left unchanged. Patients still wrestle with the same quiet fears, doubts, and uncertainties when beginning a new therapy.
The system advanced, but the human struggle remained. And that divide is now the defining challenge in adherence.
The digital promise that never materialised
Pharma’s digital-first vision made sense. We believed that if we could streamline every step of the journey, the patient experience would naturally improve with it.
But the digital-first promise carried a blind spot: it solves for tasks, not emotions. Patients don’t start, stay on, or return to therapy because they receive a notification at the right time. They stay on therapy when they feel confident, supported, and understood – none of which can be automated.
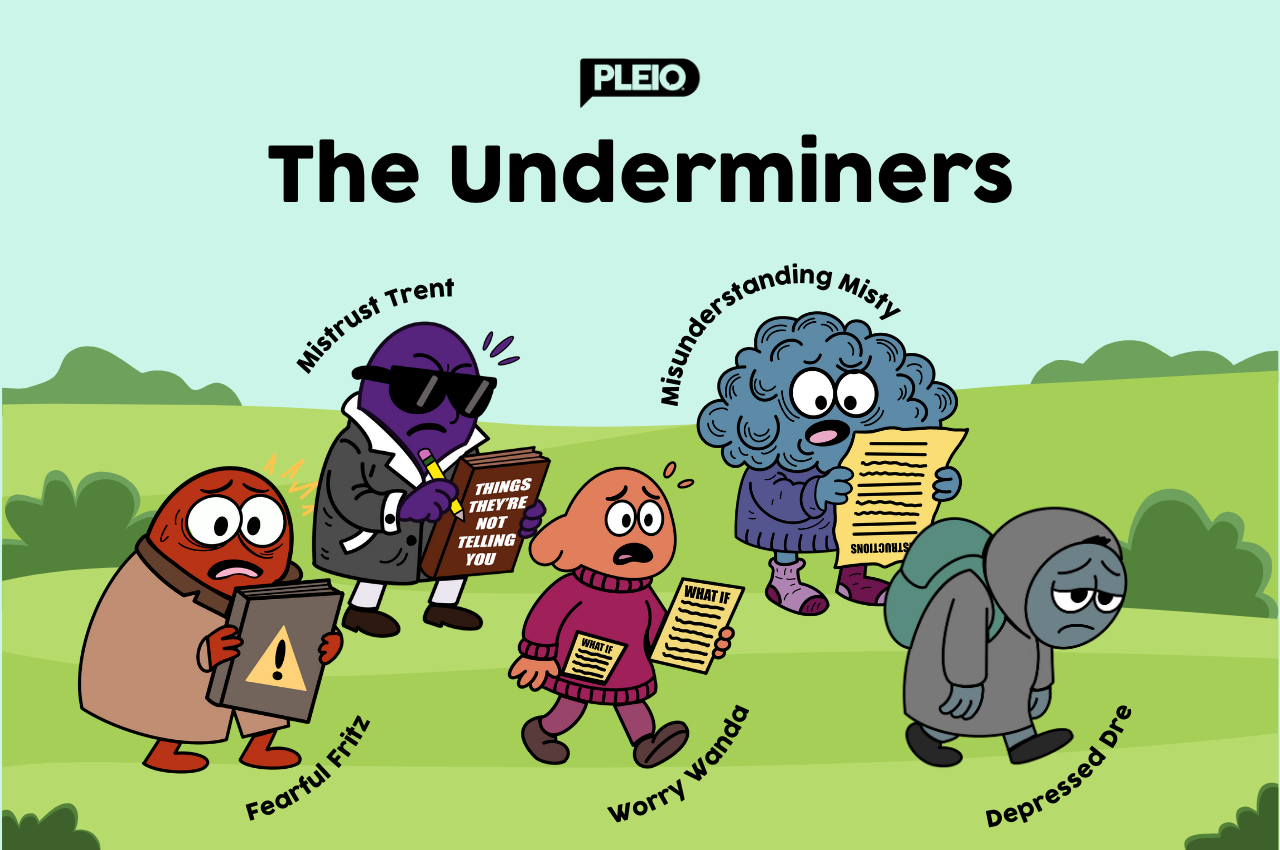
The underminers pharma must confront
In our recent analysis report of over 140,000 patient conversations, rather than ranking problems in isolation, we looked at how seven overlapping dimensions – attitudes , emotion, finance, knowledge, logistics, skills, and support – interact across 37 drivers and 85 barriers, providing a multidimensional view of adherence that reveals how complex each patient experience truly is.
A patient may express a knowledge gap, a skills gap, and an emotional concern all all at once; improving knowledge and skills is therefore only part of the solution.
These barriers are often fuelled by deeper, emotional factors such as fear, misunderstanding, mistrust, worry, and even depression. We call these the Underminers: the human states that quietly weaken confidence and disrupt the behaviours needed to start and stay on therapy. They appear across diseases, demographics, and treatment types, revealing that the real barriers to adherence are overwhelmingly human, not technical.
Behavioural science reinforces this truth. Daniel Kahneman’s Nobel Prize–winning work shows that, while people believe they act rationally, most decisions are driven by emotion and bias, not logic. The adherence journey mirrors this: patients weigh perceived benefits against perceived risks, and if negative emotions dominate, intentional non-adherence emerges. Even patients who intend to adhere can be derailed by external barriers that overwhelm their emotional bandwidth. This is why education alone rarely changes behaviour – because the decisive moment happens in the emotional mind, not the rational one.
AI can predict behaviour in 2026, but only humans can do something about it
In 2026, pharma will face a hard reality: knowing a patient may struggle is not the same as helping them change. Digital-first tools can forecast risk, surface patterns, and automate workflows, but they cannot change the emotional realities driving patient decisions. If the industry wants a different outcome, it must embrace a different model – one where technology sharpens our understanding of patients, and humans shape what happens next.
In this model, AI does what it does best: identify behavioural patterns, detect emotional signals, personalise communication and strip away administrative burden. It reveals why a patient might hesitate and when support is needed most.
But only humans can do the rest. Only a real person can interpret the nuance behind a patient’s hesitation, rebuild trust after a difficult experience, or guide someone through the fear that comes with starting a new therapy. These are moments where reassurance matters more than information and connection matters more than efficiency.
Pharma’s future splits here: Understand patients, or lose them
Pharma’s digital revolution built impressive systems. But systems don’t take medicine, people do. And people make decisions for reasons that are emotional, relational, and deeply human.
As we approach 2026, the path forwards is clear. Pharma must stop treating adherence as a workflow problem and start recognising it as a human one. AI will give us unprecedented visibility into why patients struggle, but only humans can respond in ways that create trust, confidence, and lasting behaviour change.
Adherence will finally shift when we combine the intelligence of our systems with the empathy of our people. The future belongs to pharma teams that understand both.
About the author
 Michael Oleksiw is a corporate entrepreneur with more than 20 years of experience developing innovative products and solutions. Throughout his diverse career, he has hand-crafted bicycles, commercialised software for clinical trials, launched groundbreaking CME technologies for doctors, and introduced leading fashion technology products to the world’s top brands. As CEO of Pleio, Oleksiw has spent the last decade advancing frictionless, personalised solutions to support patients in their medication journeys.
Michael Oleksiw is a corporate entrepreneur with more than 20 years of experience developing innovative products and solutions. Throughout his diverse career, he has hand-crafted bicycles, commercialised software for clinical trials, launched groundbreaking CME technologies for doctors, and introduced leading fashion technology products to the world’s top brands. As CEO of Pleio, Oleksiw has spent the last decade advancing frictionless, personalised solutions to support patients in their medication journeys.











