Behavioural science + medical education: a transformative combination?

Behaviour change is difficult - and not least in medicine. In a world where rapid results are expected, the adoption of treatment guidelines is measured in years and medical education can have limited impact on accelerating this practice change.1
In view of this challenge, it is not surprising that behavioural science was regarded as critical to the future success of healthcare in a recent survey of over 100 pharmaceutical/healthcare professionals by McCann Health and pharmaphorum. This reflects a growing awareness of the science of human behaviour and how we make decisions—both with intuition (‘system 1’) and with reasoning (‘system 2’). Yet there is currently limited and inconsistent application of behavioural science in medical education, and a reluctance to discuss the topic in the context of education, despite the positive impact on patient outcomes.
Why should behavioural science be integral to any medical education programme?
Any medical education programme should be built on a deep understanding of HCPs and patients; this means insight into behaviours, attitudes and beliefs.
‘We need to walk in the shoes of HCPs and patients, understand their environment, motivations and challenges if we are to design effective programmes that improve health outcomes.’
The ultimate purpose of medical education is to improve patients’ lives by helping translate evidence to clinical practice (‘activation of evidence’).
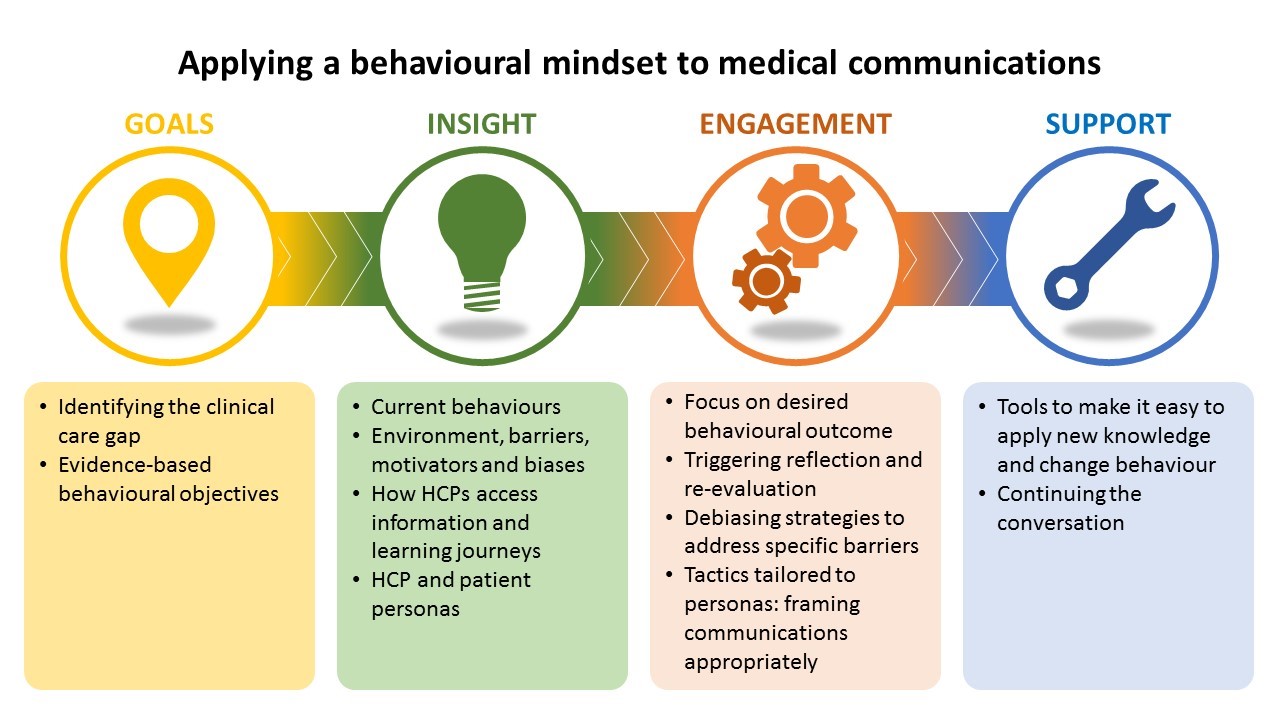
In most areas of healthcare, there is a discrepancy between what happens in clinical practice and the latest clinical data—a clinical care gap. Accelerating change is fundamentally a behavioural challenge, and to develop effective education, we need to understand the drivers of current behaviour. Then we can develop programmes that address the barriers and harness the enablers to evidence-based clinical practice.
How do HCPs and patients live their lives and make decisions?
We need to get to the heart of the decision-making process by applying a behavioural lens to gain insight into the perspective of both HCPs and patients and the dynamic of their interactions. The environment, internal (current beliefs, existing knowledge) and external (peer influence, time pressures) factors, trusted information sources and preferred channels build a holistic picture of how they live their lives—emotionally, socially, culturally and technologically.
This behavioural picture unveils the drivers and barriers to evidence-based clinical decisions that provide a focus for communications. For example, in many disease areas, HCPs tend to have a few common diagnoses at front of mind at the beginning of a patient consultation. This intuitive ‘system 1’ thinking can result in failure to consider alternatives and in premature diagnostic closure. Biases such as this are common barriers. Two universal issues in healthcare are the reluctance to give up tried and trusted management approaches (a consequence of loss aversion and other biases) and the prioritisation of short-term/immediate outcomes over the long term.
‘We are biased towards the status quo and short-term benefits rather
than long-term outcomes.’
Another common theme is the discrepancy between HCP and patient perspectives—for example, a difference in objectives for treatment or the reluctance of an HCP to engage in a ‘difficult’ discussion because of past experiences or lack of adequate management options. For example, most pharmacological treatments in major depressive disorder (MDD) address mood. HCPs are familiar with this focus, but an unconscious outcome of this familiarity is that cognition, another important aspect of MDD, is less likely to be considered when treating patients.
It is overly simplistic to view HCPs and patients as homogeneous groups behaviourally. HCP and patient personas, which summarise distinct behaviours, including how they engage with information sources, are useful tools to guide the development of multichannel communication tactics.
How should we design interventions to drive and maintain real change?
However compelling the evidence, it is unlikely to be actioned unless there is specific focus on addressing the behavioural barriers to evidence-based practice.
‘Simply communicating clinical evidence is by itself insufficient to change behaviour.’
In the previous MDD example, this requires tactics to move HCPs from their embedded intuitive (‘system 1’) response, to encourage reflective thinking (‘system 2’) and to embolden them to think about addressing other aspects of the disorder, such as cognition. This debiasing is a common approach and relies upon initially appealing to ‘system 1’ with appropriate triggers and framing; for example, these might be emotive case studies, a provocative question or an immersive app. Initial engagement by appealing to ‘system 1’ provides a springboard to engage logical reasoning through ‘system 2’ and critical evaluation of the evidence and its practical implications.
‘Behaviour change is not certain to result from new knowledge
and an intent to act.’
Individual interventions are unlikely to achieve sustained behaviour change, and part of the solution is a longitudinal programme of engagement tailored to the HCP/patient personas. However, the question ‘How do I apply this new knowledge?’ often remains. To increase the likelihood of change, additional tailored tools (such as disease assessment tools or mnemonics) should be implemented to make it easier to adopt the new behaviour.
What are the golden rules for effective and affective communication?
Whilst we have focused on understanding and addressing the specific behavioural context for medical education, there are some basic behavioural science principles to apply than can increase effectiveness of any communication. Amongst the simplest approaches is EAST, a model developed by the UK government’s Behavioural Insights Team.2 Critically evaluating a communication to ensure that it is Easy, Attractive, Social and Timely ensures that universal barriers to change are minimised and common enablers are harnessed to support change.
What benefits does a behavioural mindset bring to medical education?
A behavioural mindset can transform medical education by providing laser focus on the end goal. It reframes thinking to define educational objectives in behavioural terms, to understand how HCPs and patients think and to apply this knowledge in tactics tailored to maximise the likelihood of positive behaviour change. It is about smarter, more effective communication, not more communication—something that is increasingly relevant in a world of information overload.
References
- Hagen B et al. Time course of change in prescription behaviour after targeted continuing medical education in a closed loop system of repeated standardised documentation and feedback. Journal of European CME 2014, 3: 24697.
- EAST: four simple ways to apply behavioural insights. The behavioural insights team, 2014. Available at: http://www.behaviouralinsights.co.uk/wp-content/uploads/2015/07/BIT-Publication-EAST_FA_WEB.pdf.
About the author
Robert Poole (PhD) is Director of Scientific Services at Complete HealthVizion, a McCann Health company. He is highly experienced in working collaboratively with healthcare clients to transform innovative science into communication programmes that empower healthcare professionals to improve patients’ lives.











