PHTI delivers its verdict on DHTs for opioid use disorder

An evaluation of digital health technologies (DHTs) for opioid use disorder (OUD) by the Peterson Health Technology Institute (PHTI) has found they are as effective as regular care, but don't expand access and may increase the cost of care.
The latest in a series of deliberations on DHTs by the health technology assessment (HTA) body found that virtual technologies for OUD can help people stay in treatment slightly longer – around 13 more days over six months than usual care with drug therapies sometimes combined with counselling and recovery support.
On the other hand, PHTI found no evidence that these solutions improve access to care by increasing the number of patients who are newly entering treatment. And, given that treatment retention is thought to be the critical factor for helping people with OUD avoid overdose and hospital admissions, the report concludes that they do not substantially reduce healthcare spending on OUD and "may increase costs, depending on […] price."
Its assessment covers medication-focused (MOUD) software and 'digital wraparound solutions' used to enhance MOUD treatment programmes by adding support services.
It evaluated products from 16 companies in the MOUD category, from Affect Therapeutics, Aware Recovery Care, Better Life Partners, Bicycle Health, Boulder Care, Eleanor Health, Groups Recover Together, Ophelia, Pelago, PursueCare, Wayspring, and Workit Health.
Meanwhile, in the digital wraparound category were four DHTs from CHESS Health, DynamiCare Health, Q2i, and WEconnect Health.
The potential for raising costs is greater with the latter category, according to PHTI, based on an assumption that they cost around $200 per month per user.
"When it comes to [OUD], any additional time in treatment helps patients avoid relapse and overdose risk," commented Caroline Pearson, executive director of PHTI.
"Virtual solutions perform as well as or slightly better than traditional care models, but healthcare providers and digital solutions need to continue striving for interventions that deliver more substantial improvements in retention and effectiveness," she added. "In the meantime, the biggest impact for these solutions is to expand adoption to previously untreated patients who can benefit from proven medications and desperately need the help."
OUD is a major public health crisis in the US that resulted in approximately 80,000 deaths from overdose last year and is associated with an estimated $111 billion in direct healthcare costs every year.
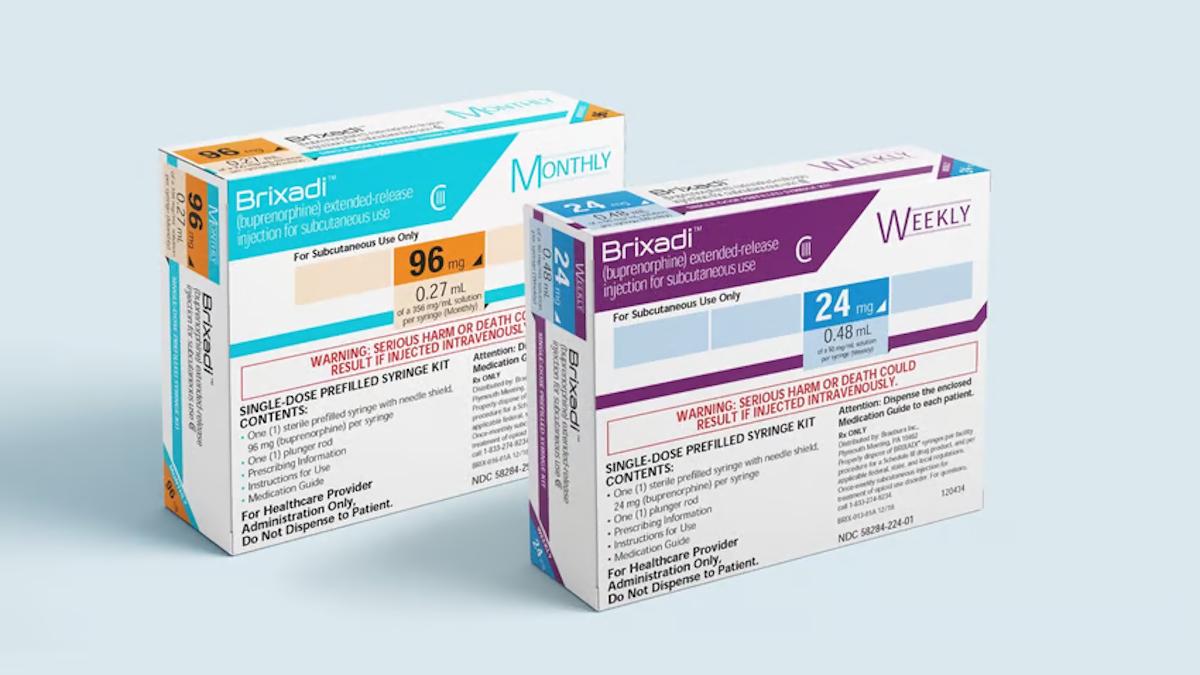
Despite the efficacy of drugs like buprenorphine, methadone, and naltrexone, only around a quarter of adults in need of OUD treatment get medication-based treatment, a situation that has been blamed in part to a lack of access to care providers, one area that DHTs are designed to address.
PHTI's OUD report comes after earlier assessments of DHTs for depression and anxiety, hypertension, musculoskeletal disorders, and diabetes, with another on gastrointestinal diseases in the works.