PHTI backs virtual therapies for musculoskeletal disorders
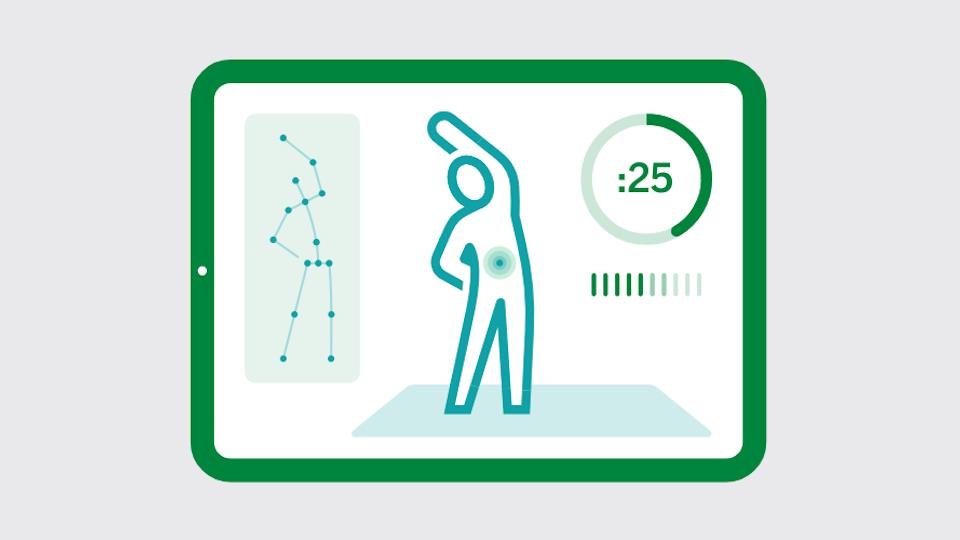
A new report from the Peterson Health Technology Institute has concluded that many digital therapies for musculoskeletal (MSK) conditions like low back pain can deliver clinically meaningful benefits in pain and function.
The analysis from the health technology assessment (HTA) organisation concludes that they offer clinical benefits to patients that are comparable to in-person physical therapy (PT) and should be included in medical benefits insurance as they have the potential to “ improve access to therapy, reduce healthcare spending, and offer greater convenience” to patients.
The report covered exercise therapy apps Dario and Kaia, virtual physiotherapist-guided tools Hinge, Omada, RecoveryOne, Sword, and Vori, and Limber, a remote therapeutic monitoring (RTM) physiotherapy programme.
The exercise therapy apps improved pain but did not have much impact on function, and according to PHTI were not substitutable for in-person PT although they could be useful – depending on price – for less serious MSK disorders. Limber scored well and may even outperform in-person PT alone, it said, but its price leads to a net increase in healthcare spending.
The PT-guided solutions were in the sweet spot of improving pain and function and reducing net spending, mainly from avoided care, and PHTI said the evidence supports broader adoption. Purchasers and providers should encourage more PT-first MSK care, it added.
“We know that early and regular use of physical therapy can speed the healing process and avoid other complex MSK care, such as surgery,” said Caroline Pearson, executive director of PHTI.
“Our findings indicate that virtual solutions represent effective treatment options that can expand the number of patients who both start and stick with physical therapy,” she added. “In order to realise their full potential, virtual MSK solutions should be more closely integrated with medical care and insurance benefits.”
The MSK study has a much more positive verdict than PHTI’s earlier report on digital tools to help people with diabetes manage their blood sugar levels, which concluded that they provide little benefit and add to healthcare spending.
The body – which is affiliated with the Institute for Clinical and Economic Review (ICER) that conducts cost-effectiveness assessments on prescription medicines sold in the US market – was set up to test the claim that 80% of digital health products lack clinical evidence.
It is also casting its eye over digital hypertension and depression/anxiety tools, with verdicts expected later this year.
PHTI is running a free webinar next week (13th June) to discuss the MSK report’s findings.













