AI picks up interval breast cancers missed by scans
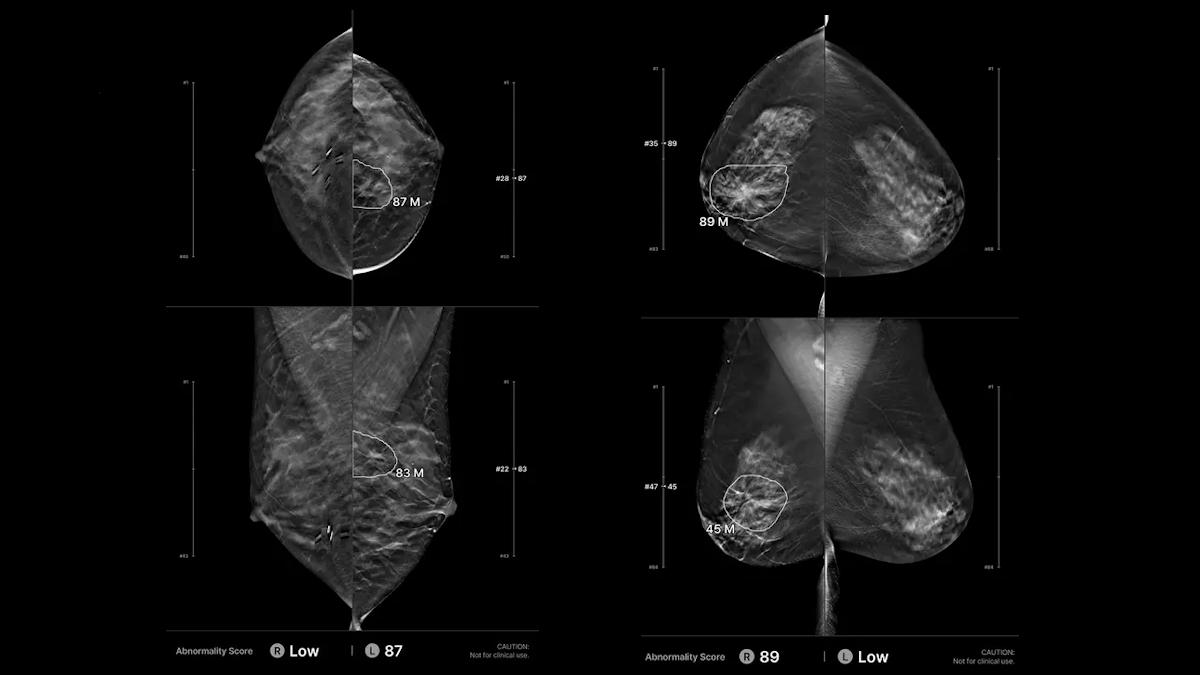
Examples of positive and false positive results with the Lunit AI
An AI algorithm has been shown to improve the diagnosis of interval breast cancers, tumours that are diagnosed between routine screening appointments, when used on top of regular scans.
The algorithm, developed by AI specialist Lunit, was retrospectively tested in conjunction with an advanced 3D mammography technology known as digital breast tomosynthesis (DBT) in 224 cases of interval breast cancer among women who had this type of screening.
Lunit INSIGHT DBT correctly identified nearly a third (32,6%) of cancers that were previously undetected, according to the study, which has been published in the journal Radiology.
The algorithm correctly localised 84.4% of 334 true-positive cancers, and correctly categorised 85.9% of 333 true-negative cases and 73.2% of 333 false-positive cases as negative.
Interval breast cancers, found in the three-year gap between a normal result and before the next screening appointment, are notoriously hard to manage because they tend to be aggressive and rapidly growing. In some cases, they occur between the scans, but in others they are present already, although so small they are hard to detect.
In England alone, each year approximately 6,000 women in the breast screening programme will develop an interval cancer, according to the NHS.
DBT is a relatively new technology, so is not yet widely used – in the UK, for example, it can only be used in the context of clinical trials – but it has been shown to improve the visualisation of breast lesions and reveal cancers that may be obscured by dense tissue.
In the US, the technology is more widely deployed, although, that has taken place relatively recently and there remains a lack of data on patient outcomes. The new study is one of the first to specifically examine AI assistance in detecting interval cancers on screening DBT exams.
"Given the lack of long-term data on breast cancer-related mortality measured over 10 or more years following the initiation of DBT screening, the interval cancer rate was often used as a surrogate marker," said study author Manisha Bah, breast imaging division quality director and co-service chief at Massachusetts General Hospital.
"Lowering this rate is assumed to reduce breast cancer-related morbidity and mortality," she added. "My team and I were surprised to find that nearly one-third of interval cancers were detected and correctly localised by the AI algorithm on screening mammograms that had been interpreted as negative by radiologists."
Cancers detected by the algorithm tended to be larger, and they were more likely to be lymph node-positive, according to Bahl.
"These findings suggest that AI may preferentially detect more aggressive or rapidly growing tumours, or that it identifies missed cancers that were already advanced at the time of screening," she said.
The results suggest the algorithm should be incorporated into radiology workflows, according to the researchers, although, they note in the paper that its effectiveness will still need to be assessed and validated in real-world settings.












