Shifting paradigms of clinical trial design accelerate CNS R&D
Meeting the demand for clinically relevant neurodegenerative treatments requires a paradigm shift in how central nervous system (CNS) clinical trials have been designed and executed. Four years ago, in 2021, Alzheimer’s disease was estimated to affect 56,900,000 people, globally – a 160% increase from 1990.1 Meanwhile, research into Alzheimer's treatments was unsuccessful, with an attrition rate of nearly 100% for phase II and III Alzheimer’s trials between 2003 and 2022.2
However, within the last five years, the landscape appears to have shifted. In June of 2021, the first disease-modifying treatment for Alzheimer’s, aducanumab, achieved conditional approval. Since then, other amyloid-targeting monoclonal antibodies, lecanemab and donanemab, have been approved by the US Food and Drug Administration (FDA) for early Alzheimer’s disease.3
Importantly, the approved molecules for Alzheimer's disease came from a drug class that was tested and failed 15 years prior. The successful Alzheimer's trials were primarily distinguished from preceding trials of similar compounds because they employed more accurate and sensitive biomarkers, which allowed for treatment of more correctly diagnosed patients earlier in their disease.
Buoyed by the breakthrough technologies and methodologies that have enabled earlier intervention, Alzheimer’s drug developers are now at the forefront of adopting more nuanced, cost-effective, and patient-centric clinical trial designs. For example, an ongoing study of lecanemab (AHEAD 3-45) in pre-symptomatic stage patients is one of the first neurodegenerative trials to focus on “asymptomatic patients”, and uses several innovative designs and technologies to accelerate and de-risk clinical development. These include registry-based patient enrichment, blood-based biomarker screening, individualised dosing, and parallel trials assessing distinct disease subpopulations.4 Though the trials have not concluded, the clinical trial sponsors have already published their trial design methods, along with some promising interim results.5
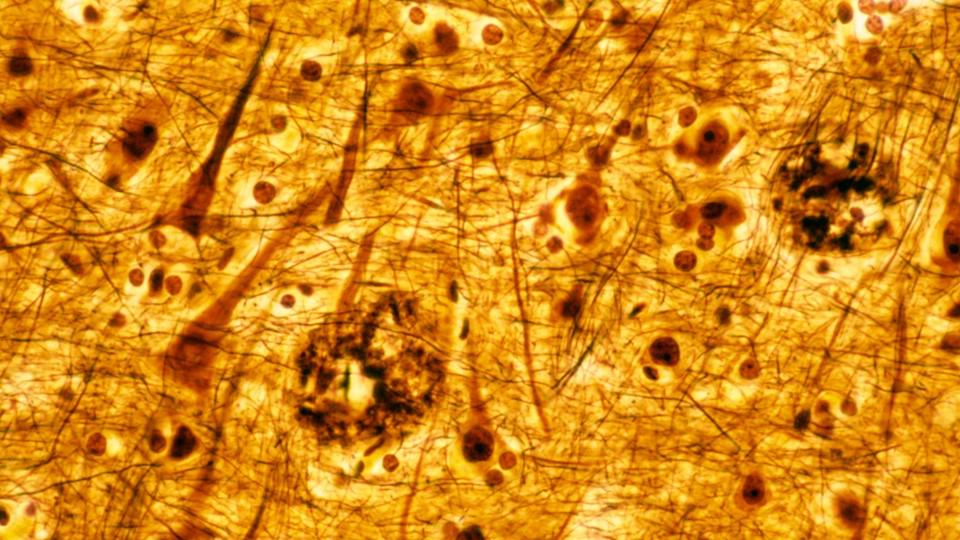
Models for success in Alzheimer’s could have far-reaching implications, because they address common challenges with disease complexity, trial design, and execution that underlie the high rates of failure in neurodegenerative clinical development. For many neurodegenerative diseases, including Alzheimer’s, changes in the brain begin years before clinical signs of disease emerge.
Clinical symptoms start out mild and non-specific, gradually worsen, and vary between individuals. Up to three in four of symptomatic Alzheimer’s patients are misdiagnosed or undiagnosed in primary care.6 And correct diagnosis often occurs late in disease progression after quality of life is impacted, when damage to the brain may be extensive, and possibly irreversible.7 High rates of delayed diagnosis and misdiagnosis are challenging for patients and contribute to clinical trial failures.
Given the shared challenges with diagnosis and outcomes assessment, CNS developers are watching trailblazing Alzheimer’s clinical trials with renewed optimism for other diseases, and clinical development paradigms for the broader spectrum of neurodegenerative diseases are shifting. To determine the extent to which advances, such as blood-based biomarkers, digital health technologies, and non-traditional trial designs, are being applied today, ICON surveyed 129 CNS therapeutic developers focused on neurodegenerative disease.
Emerging biomarkers improve patient screening and outcomes assessment
Overall, the survey suggested an exceptional uptake of biomarkers in CNS clinical trials, with 97% of respondents adopting them. The level of biomarker adoption for patient screening (57%) was consistent with its use for outcomes assessment. High levels of biomarker adoption for patient screening reflects the potential of biomarkers to more accurately diagnose patients earlier in the course of a neurodegenerative disease when compared to diagnosis based on clinical symptoms. This, in turn, reduces the burden of misdiagnosis on patients and clinical trials.
Recently developed blood-based biomarkers now offer more accessible alternatives to traditional biomarker-based diagnostic methods, which relied on imaging machines or spinal taps. Adoption of more accessible biomarkers has been rapid, with respondents reporting the use of non-CSF (cerebrospinal fluid) based bio-fluid biomarkers more often than any other modality (56%).
Biomarkers are also invaluable in outcomes assessment. Digital biomarkers, in general, and wearable sensors, in particular, have exciting potential to collect data on cognitive function, motor symptoms, and other relevant disease features. This provides objective, continuous data, improving sensitivity and decreasing data variability.
Ideally, digital biomarkers can also reduce patient burden, by enabling less burdensome methods of outcomes reporting. In turn, more accessible methods of outcomes assessment can help to ensure patient engagement throughout a trial, and improve compliance. Wearables are most commonly used in neurodegenerative diseases with motor-based symptoms, such as Parkinson-type syndromes.
However, the selection and adoption of biomarkers must be strategic, with considerations for how selected biomarkers will impact every stage of clinical development and commercialisation. When selecting biomarkers, sponsors should make sure that any biomarker-based inclusion criteria and outcomes assessment methods are validated across patient populations, and reflect clinical changes that are meaningful to patients.
In Alzheimer’s, lower average levels of amyloid in black individuals have resulted in lower eligibility of these individuals in some Alzheimer's clinical trials.8 Biomarkers, such as the ratio of plasma Aβ42/40, which has demonstrated more consistency across racial groups, may help streamline and accelerate the enrolment of representative patient populations.9 Developers using digital biomarkers for outcomes assessment should also be aware that few are FDA approved or acceptable as primary endpoints in pivotal trials. So, validation and justification of digital health technologies is crucial.
Non-traditional trial designs improve feasibility and efficiency
While recent biomarker innovations have enabled earlier and more accurate enrolment of patients with neurodegenerative diseases, implementing biomarker-based screening could also increase the cost and duration of clinical trial recruitment, particularly if eligible patients have limited access to screening or if screen-fail rates rise. This could exacerbate already considerable challenges faced with recruitment and retention of qualified, diverse patients reportedly experienced by over 80% of CNS developer survey respondents.
Non-traditional trial designs can help improve the feasibility of biomarker-based screening by accelerating patient recruitment and contributing to cost savings in clinical development. Studies, such as AHEAD 3-45, have demonstrated that recruiting from registries of trial-ready cohorts majorly accelerates enrolment of qualified patients, and is an enormous asset to clinical developers, especially those conducting trials in early disease patients or with biomarker-based eligibility requirements.
With less than a third of survey respondents utilising registries or non-interventional trials, these recruitment strategies are a surprisingly underutilised way to improve the drug development process for neurodegenerative conditions. That may be because of the high resource requirements for such a huge registry. More targeted concepts, which are closely aligned with the interventional trial and that rely on remote screening tools, may still provide pre-symptomatic, enrolment-ready cohorts at lower costs.
Sponsors may also address challenges with recruitment and retention of enough individuals through the implementation of platform trials, which allow for a trial to enrol patients on a rolling basis, or historic controls, which allow all active patients to be enrolled in treatment groups. These trial design methods also appear to be underutilised. In the survey, less than a quarter of respondents reported using historic controls (22%) or platform trial designs (19%).
Overall, survey trends of adoption and application suggest that across the board, the way that CNS clinical trials are designed and executed is shifting to accommodate the adoption of biomarkers for patient enrolment and outcomes assessment. However, non-traditional trial designs that support the use of biomarker-based diagnosis, screening, and outcomes assessment remain underutilised. Importantly, the way new technologies are applied and accounted for in CNS trial design will determine whether they can fulfil their promise to accelerate and de-risk research and development across the full spectrum of CNS diseases.
About the author
 Bill Holt, DO, is vice president of drug development solutions, neurology, at ICON.
Bill Holt, DO, is vice president of drug development solutions, neurology, at ICON.
References
1. Steinmetz JD, Seeher KM, Schiess N, et al. Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024;23(4):344-381. doi:10.1016/S1474-4422(24)00038-3
2. Kim CK, Lee YR, Ong L, Gold M, Kalali A, Sarkar J. Alzheimer’s Disease: Key Insights from Two Decades of Clinical Trial Failures. J ALZHEIMERS Dis. 2022;87(1):83-100. doi:10.3233/JAD-215699
3. Cummings J, Zhou Y, Lee G, Zhong K, Fonseca J, Cheng F. Alzheimer’s disease drug development pipeline: 2024. Alzheimers Dement Transl Res Clin Interv. 2024;10(2):e12465. doi:10.1002/trc2.12465
4. Rafii MS, Sperling RA, Donohue MC, et al. The AHEAD 3-45 Study: Design of a prevention trial for Alzheimer’s disease. ALZHEIMERS Dement. 2023;19(4):1227-1233. doi:10.1002/alz.12748
5. Pugh MAM. TRAILBLAZER-ALZ 3 – A Deeper Dive into Time-to-Event Trials. Alzheimers Dement. 2023;19(S21):e070865. doi:10.1002/alz.070865
6. Hansson O, Edelmayer RM, Boxer AL, et al. The Alzheimer’s Association appropriate use recommendations for blood biomarkers in Alzheimer’s disease. ALZHEIMERS Dement. 2022;18(12):2669-2686. doi:10.1002/alz.12756
7. Dubois B, von Arnim CAF, Burnie N, Bozeat S, Cummings J. Biomarkers in Alzheimer’s disease: role in early and differential diagnosis and recognition of atypical variants. Alzheimers Res Ther. 2023;15(1):175. doi:10.1186/s13195-023-01314-6
8. Molina-Henry DP, Raman R, Liu A, et al. Racial and ethnic differences in plasma biomarker eligibility for a preclinical Alzheimer’s disease trial. Alzheimers Dement. 2024;20(6):3827-3838. doi:10.1002/alz.13803
9. Xiong C, Luo J, Wolk DA, et al. Baseline levels and longitudinal changes in plasma Aβ42/40 among Black and white individuals. Nat Commun. 2024;15(1):5539. doi:10.1038/s41467-024-49859-w