Wearables still lack evidence of patient outcomes

The idea that wearable biosensors could help revolutionise healthcare by providing real world data has been around a while - but proof that they help patients is yet to emerge.
A new study by investigators from Los Angeles' Cedars-Sinai Hospital, writing in the Nature journal, npj Digital Medicine conducted a literature analysis and found that remote patient monitoring with these sensors had no statistically significant impact on any of six clinical outcomes studied: body mass index, weight, waist circumference, body fat percentage, systolic and diastolic blood pressure.
[caption id="attachment_36249" align="alignnone" width="180"] Brennan Spiegel[/caption]
Brennan Spiegel[/caption]
Led by senior author Brennan Spiegel, the study found these devices had shown promise in improving outcomes for conditions, such as COPD, Parkinson's disease, hypertension and low back pain.
But Spiegel said: "As of now, we don't have enough evidence that they consistently change clinical outcomes in a meaningful way."
Investigators conducted a statistical analysis and in-depth literature review of 27 studies from 13 countries published between January 2000 and October 2016. Each study examined the effects of remote patient monitoring using wearable biosensors.
The interventions targeted patients who were overweight or suffering from heart disease, lung disease, chronic pain, stroke or Parkinson's.
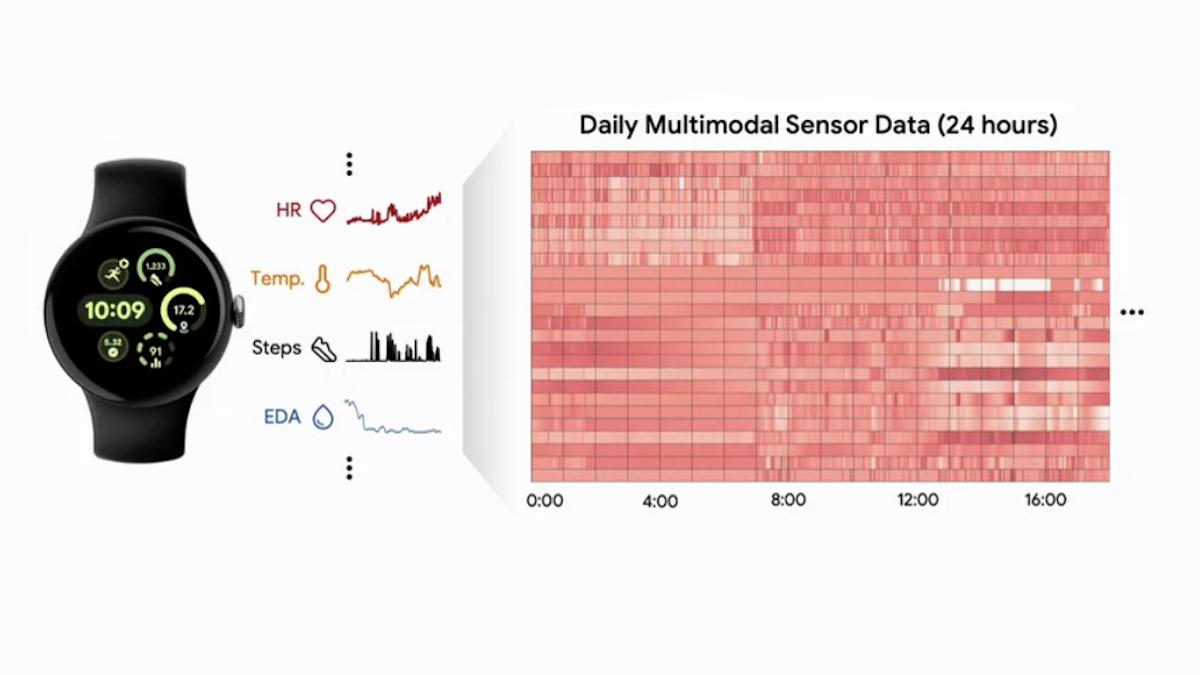
The devices studied included physical activity trackers, blood pressure monitors, electrocardiograms, electronic weight scales, accelerometers (devices measuring acceleration) and pulse oximeters (oxygen saturation monitors), among others. These devices were embedded in everything from watches and belts to skin patches and textiles.
A statistical analysis revealed that remote patient monitoring resulted in no significant impact on any of the reported clinical outcomes.
Certain types of interventions worked best, including efforts grounded in social science models and established care guidelines and those that used personalised coaching.
Only 16 out of 4000 studies were high quality
Authors concluded that there was a lack of data from study evidence provided so far.
Of more than 4,000 studies the authors initially reviewed, fewer than 1% were eligible to be included in the study, and only 16 were considered high-quality research. The authors found very few randomised controlled trials for each of the clinical outcomes analysed, and studies varied significantly in terms of the types of devices used, the populations studied and the interventions tested.
"Many of the studies we reviewed were still in the pilot phase," said lead author Benjamin Noah, a clinical research associate at the Center for Outcomes Research and Education. "There just is not enough data yet."
More robust trials are likely to be on their way, however, as many pharmaceutical companies are now exploring their use in proof-of-concept trials.
In June last year Parexel and Sanofi announced they would undertake research to find out just how useful wearables are for patients and investigators in a clinical trial setting. This of course differs from use of wearables in the real world, where monitoring and compliance is more problematic.
Photograph courtesy of Cedars-Sinai Hospital