Cheaper gene modifying process could cut CAR-T costs
CAR-T cancer therapies are notoriously expensive – with the first approved drugs costing hundreds of thousands of dollars per patients.
The headline price of ‘living drugs’ or chimeric antigen receptor T-cell (CAR-T) therapies has created controversy – but it’s a fact that harvesting a patient’s T-cells, genetically modifying them to attack cancer, and injecting them back into the body, is an expensive endeavour.
While there are substantial costs at each part of the process, a significant tranche comes from genetically engineering the cells, and this is having an impact not just on the headline cost of drugs, but also the cost of early-stage research into potential new CAR-Ts.
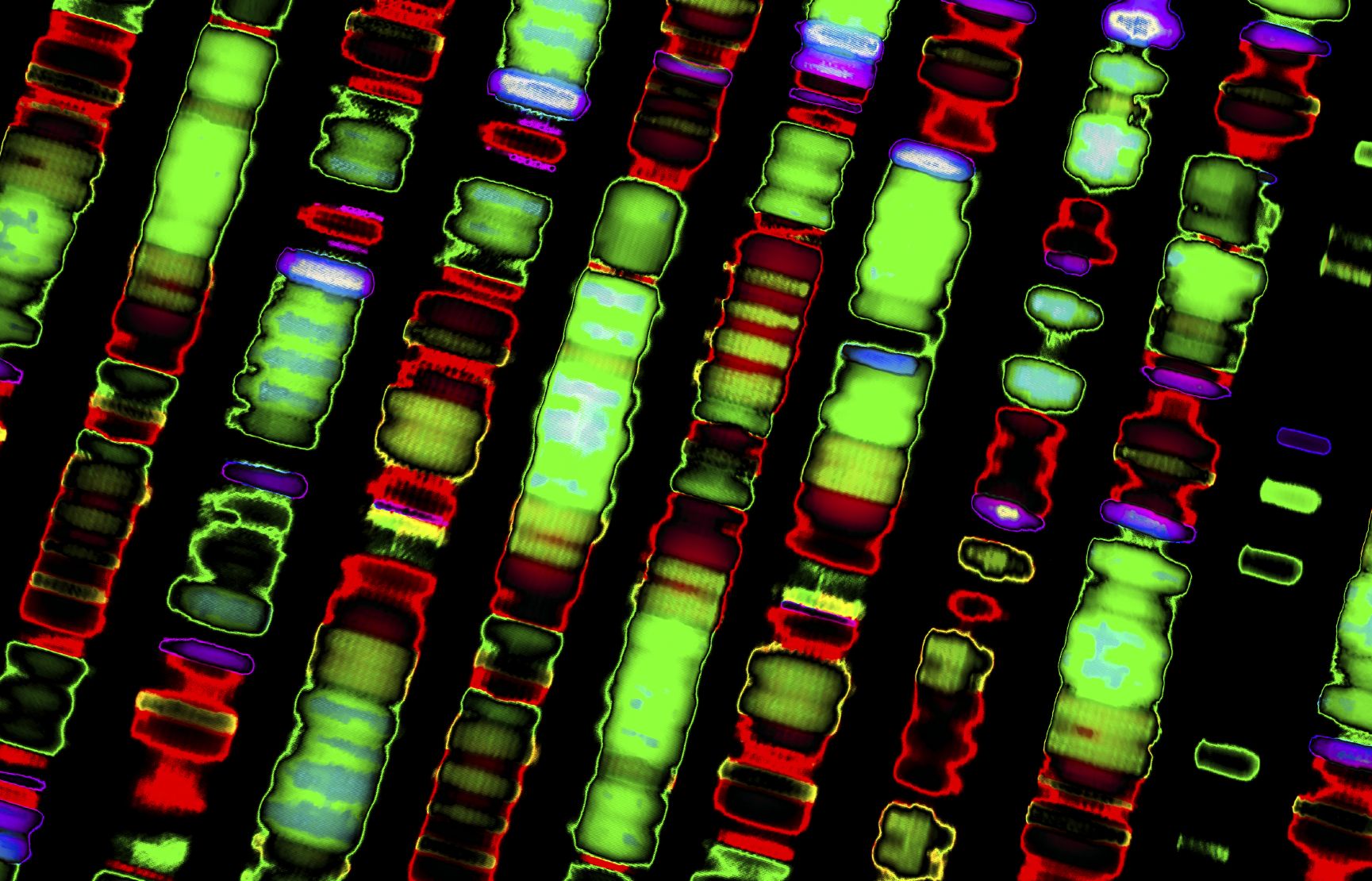
The approved CAR-T therapies use a lentiviral vector to genetically engineer the cells – a modified virus that injects the gene into the harvested T-cells, causing them to express the cancer-killing receptor.
Setting up a process such as that developed by Oxford Biomedica, based around a modified HIV virus, requires a large amount of cash.
The UK biotech is now seeing a return on its investment with a lucrative licensing deal after Novartis chose it to make the vectors needed for its CAR-T, Kymriah (tisagenlecluecel).
But it is more difficult to cost-effectively make production of vectors for smaller CAR-T trials using this technology - so the search is on for alternative ways to genetically engineer the cells.
Speaking at Kisaco Research’s Combined CAR-T Congress in Berlin, professor Dr Zoltan Ivics, medical biotechnology head of division at the Paul-Ehrlich-Institut in Langen, Germany, said one alternative is the process known as ‘Sleeping Beauty” non-viral engineering.
This involves using DNA-based vectors known as minicircles, which unlike plasmids contain no bacterial DNA sequences and are much less likely to be perceived as foreign and to be destroyed when introduced into a cell.
Ivics said that scientists have been working on improving this technology over the last few decades, and it is now efficient enough for commercial use, either in research, or in future marketed products.
They can be produced at 10% of the cost of a viral vector that complies with regulatory restrictions, with powerful implications for small scale trials and early research.
Using this kind of vector would benefit smaller research outfits that are attempting to find new CAR-T therapies, said Ivics.
The process is also fast, taking around a week as opposed around four weeks with virus vectors.

Zoltan Ivics
Ivics said: “Small research groups shy away from clinical trials [of CAR-Ts] without this option.”
“It is a very important asset now that the proof of concept is out there, to democratise this research.”
“It is an extremely strong option for phase 1 development, especially phase 1 development, many companies could benefit.”
There are drawbacks however – transfer efficiency drops off if genes are longer than 10,000 base pairs, although it is possible to transfer genes of up to 100,000 base pairs.
However he noted that only a small quantity of vector is needed for trial purposes. He added that the process could also produce enough vector to reduce the cost of producing a CAR-T therapy once it is approved for the market.
Ivics said: “You can have a few milligrams of GMP grade vector sitting in the freezer – that is enough for many many patients.”












