After a no in sickle cell, NICE OKs Casgevy for thalassaemia
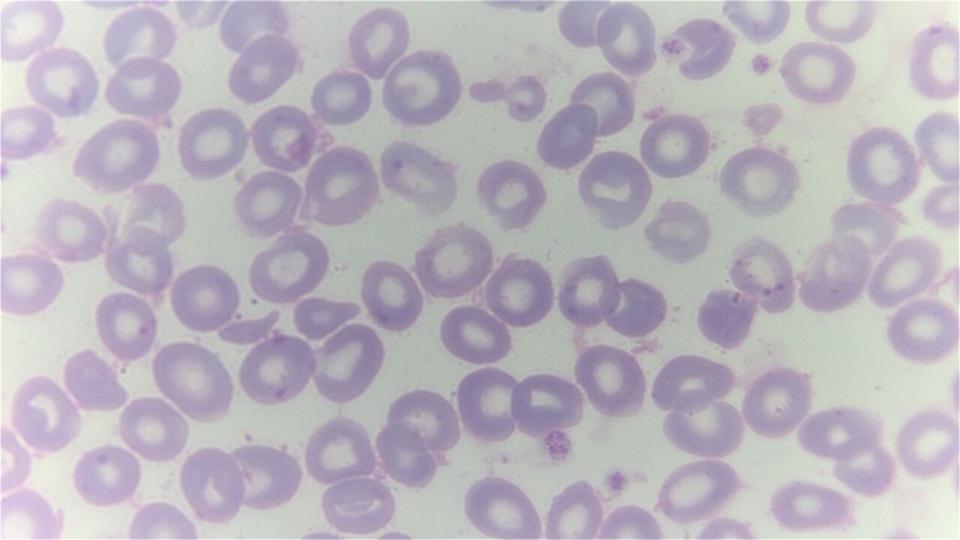
Beta thalassaemia cells
Vertex and CRISPR Therapeutics have won the backing of NICE for their gene-editing therapy Casgevy as a treatment for the blood disorder beta thalassaemia, a few months after turning it down for sickle cell disease.
Final draft guidance published this morning clears Casgevy (exagamglogene autotemcel) as an option for people 12 years and over with severe beta thalassaemia who need regular blood transfusions and for whom a blood and bone marrow transplant is advised, but no donor is available.
Casgevy was cleared by the MHRA last November as a one-shot therapy for the two indications, marking the first time any regulator had approved it for marketing. The therapy is the first based on gene-editing technology to reach the market and has since also been approved in the EU and US.
It has a list price of £1.65 million ($2.2 million) but will be provided to the NHS at a confidential discount under a reimbursement agreement with Vertex, which said securing access is "a historic moment for people living with transfusion-dependent beta thalassaemia who, for too long, have had limited options for this life-shortening disease."
Funding will come from NHS England's Innovative Medicines Fund (IMF), which temporarily foots the bill for promising medicines while additional evidence of their benefits is gathered.
It's a different outcome to NICE's earlier decision to reject routine NHS use of Casgevy in SCD in draft guidance published in March, saying it required "more information to address the uncertainties in the clinical and economic evidence."
Vertex said it is continuing to work with NICE and NHS England to ensure eligible SCD patients can also access this treatment as soon as possible.
It involves harvesting bone marrow stem cells from patients and using CRISPR/Cas9 to modify them outside the body (ex vivo) before reinfusing them to treat the diseases.
"Although there are some uncertainties in the evidence for its long-term benefits, the committee felt exa-cel could represent a potential cure for some people with transfusion-dependent beta thalassaemia, freeing them from the burden and risks of needing regular blood transfusions," said the agency's director of medicines evaluation Helen Knight.
In the UK, transfusion-dependent thalassaemia mainly affects people of Pakistani, Indian and Bangladeshi ethnic origin, according to NICE, which estimates that around 460 people could be eligible for Casgevy in England.
Dr Diana Hernandez, director of immune and advanced therapies at stem cell charity Anthony Nolan, said that people in these groups are less likely to have a tissue-type matched donor on the stem cell register, making Casgevy the only viable option.
"Casgevy offers an effective cure for transfusion-dependent beta thalassaemia for people without a stem cell donor," she added, whilst pointing out there is also a desperate need for new options in the SCD community.
"Sickle cell largely affects patients from African and African-Caribbean backgrounds, who are less likely to have a matching stem cell donor, and this community has been waiting years for a new, effective treatment."
Image by Dr Graham Beards via Wikimedia











