Israel’s MedTech and health innovation landscape: Part one – Technology & emergency responsiveness

Image by Nicole Raleigh
At the beginning of the year, this editor was invited to take part in a life sciences-specific tour organised by The Jerusalem Press Club, providing unique insight into current innovation and investment in the country: a determined attempt to exhibit the ongoing efforts behind the scenes to create better outcomes for patients – globally – despite ongoing turbulence in terms of its geopolitical climate; and despite a testing time in the spotlight of the world stage and public opinion.
This series of articles – Israel’s MedTech and health innovation landscape: From Tel Aviv to Jerusalem – will seek to share a taste of those insights gleaned during that five-day press trip. It is hoped that some small part of the truly inspiring science and resilience of these Israel-based innovators will be imparted to and spark the interest of readers.
Part One focuses on recent technological innovation in emergency responsiveness and its implementation in the health ecosystem, as seen at the Tel Aviv Sourasky Medical Center in Ichilov, as well as the Magen David Adom blood and milk bank, otherwise known as the Marcus National Blood Services Center. Subsequent articles will focus on start-up hubs, academic-industry collaborations, and venture capital opportunities, in Israel, in partnership with the US, and wider afield internationally.

Emergency medicine in action: Lessons from the trauma helipad
Dr Eyal Hashavia, director of trauma services at the Tel Aviv Sourasky Medical Center – the largest acute care facility in Israel – is a beacon of energetic preparedness for all eventualities.
A 1,500-bed, world-class governmental academic medical centre, Tel Aviv Sourasky Medical Center serves a population of one million people, including both residents from the greater Tel Aviv area and visitors to the metropolis. In 2022, the number of severely injured trauma patients admitted to the hospital was around 2,200 a year; by 2025, following the Twelve-Day War with Iran, that figure had increased to 3,800.
However, the 25-year old building stands with a helipad at its crown, and that helipad was only used perhaps once a year until 7th October 2023 and the Iron Swords War that followed.
“Believe me, on weekends, when I'm getting criminal stab wounds from Southern Tel Aviv, from the ‘nice neighborhoods of crime’, it takes them more than 15 minutes to arrive; sometimes it takes them 25 minutes [due to traffic],” said Dr Hashavia. “[But] from the far south, they come even faster than patients in Tel Aviv.”
And that is, within 15 minutes, via helicopter. After that, the helipad-to-trauma-room process – which was fine-tuned during the past two years of conflict, particularly by blast injury – sees those patients taken into the operating theatre in just three minutes. The medical centre itself is now a well-oiled machine that at any time of day or night can bring together the necessary care team of fifteen, known as the ‘Dream Team’. This, by virtue of an excellence in communications, and communicating processes.
“Our record was eight teams operating at the same time on one patient,” said Dr Hashavia. “We're just helping. We're not fixing. The body does the majority of the job. We just need to know in what order and exactly what's the magic to do in order to help the body.”

Delivering life-saving fluids, nationally and internationally
In addition to such speed and accuracy in the emergency hospital setting, the situation of the past few years has resulted in Israel becoming the first country to offer whole blood to all patients, throughout the country: “It's a game changer […] It saves lives,” as Dr Hashavia noted. But one can’t truly understand the reality and the impact of this until visiting Magen David Adom (MDA), the Marcus National Blood Services Center.
The Red Shield of David, commonly known as the Magen David or Star of David, is a significant symbol in Judaism, representing Jewish identity and heritage. After waves of immigration into the country following WWI, activists in Tel Aviv formed a rapid response first-aid organisation named after the Magen David and based on the framework of the Red Cross. The official recognition of Israel as a state in 1948 following WWII saw Magen David Adom become “a medical corps of the country,” explained Yonatan Yagodovsky, director of the Fundraising and International Relations Department of Magen David Adom in Israel.

A national, non-profit organisation largely operated by volunteers (90% of MDA’s highly trained personnel are volunteers, the other 10% are employees), the organisation is essentially Israel’s pre-hospital emergency medical system. MDA handles hundreds of thousands of life-saving cases every year, using technological devices that are among some of the most advanced in the world, in accordance with the common protocols for cardiac treatment of the American Heart Association. Indeed, the centre is the world’s first underground, shielded blood bank, designed to protect Israel’s blood supply from missile attacks, earthquakes, and cyber threats, while utilising advanced automation to process and distribute over 300,000 units annually.
“This entire building is built with different layers,” explained Yagodovsky. “There are three underground floors, but there are double floors […] It's like a, you know, matryoshka. When you walk into any bomb shelter in this building, you walk through a bomb shelter into a bomb shelter. This is an airlock, so, when there is a need, we seal both of those and then only one of the two doors can be opened.”
The centre has received many visitors from European countries due to the war in Ukraine, to see how MDA has managed to operate a secure blood service. Two-thirds of the centre underground, that nonetheless also includes a transportation department, a simulation training centre for EMTs and paramedics on a national scale, two auditoriums, and classrooms. The simulation centre, of course, employs virtual reality (VR).
“That's why the walls are green, because we can project also on the walls, in addition to what you see,” explained Yagodovsky. “Let's say we were treating people in the room over there [a ‘wet’ room that allows for rain, wind, and even chemical simulation scenarios], and now we can bring in to the ambulance, to the mobile intensive care unit, and simulate the treatment while going to the hospital. You can simulate teamwork on a patient and everything is monitored while the driver is also being tested; the team will feel his way of driving.”
A rapid-response infrastructure powered by a civilian engine
Human resources-wise, MGA trains men and women from all parts of Israeli society, Jewish and non-Jewish, and has a team of around 39,000 people.
“We work alongside the police, with firefighters, with Home Front Command and, of course, with all hospitals in Israel, all the local and regional councils all over the country,” explained Yagodovsky. “The government part in our annual budget is around 13% of our annual budget, which is mainly covering extra costs related to activities that we are asked by the government to activate in certain times […] All of our life support vehicles, this building, all of our stations […] are funded from donations from friends and supporters of Magen David Adom all over the world and within Israel.”

Magen David Adom operates 1,500 emergency vehicles and three helicopters from over 200 stations throughout the country of Israel. In 2025, the organisation marked 95 years of activity. In that year, its paramedics and EMTs were dispatched 1,383,026 times to incidents using thousands of mobile intensive care units, ambulances, emergency motorcycles, and rapid response vehicles throughout the country. On average, a call is received at MDA’s emergency dispatch centre every 7.3 seconds. The average call hold-to-response time? Up to just two seconds.
The organisation provides treatment to any individual who needs help – regardless of ethnicity, race, or political or religious affiliation – and it helps many countries during disasters, too: the earthquakes in Haiti and Nepal and tsunami victims are a few examples of international humanitarian assistance provided by MGA.
“We ask the public to come and donate blood: the Israeli public is responsible, especially in emergencies, and not only local emergencies,” noted Yagodovsky. “I still remember September 11th. People were waiting at night, 600 people donated blood in Jerusalem [alone]: ‘Maybe we will send it to New York,’ they said. And it was the time of the Intifada; we needed blood. Unfortunately, fortunately, they were managing in the hospitals in New York. There was no need to send the blood. The downside was that so many people got killed and there was no need for a massive amount of blood to be sent over.”
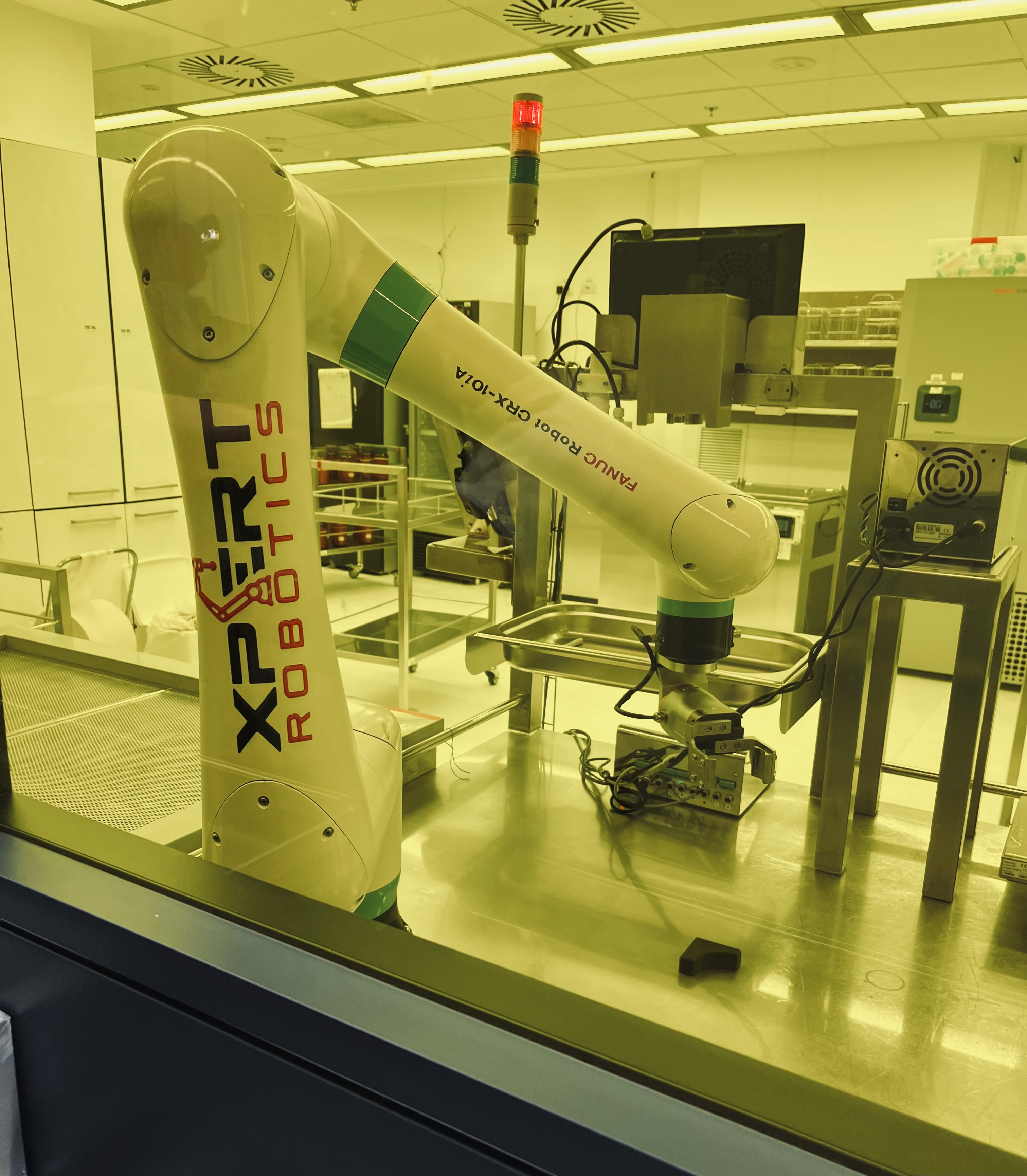
Additionally, MDA’s Human Milk Bank now supplies breast milk to premature infants in neonatal intensive care units, newborns in hospitals, and sick infants at home who require breast milk due to their medical condition. This service employs a freeze-and-collect system and robotics, and was instigated by the need of ‘war babies’ following the recent period of conflict, providing breast milk to orphans whose mothers had begun breastfeeding or wished to breastfeed and passed away after childbirth.
“We were asked by the Ministry of Health to build up a milk bank,” explained Yagodovsky. “Israel was very much behind the Western world in this type of work, and thanks to amazing women that forced the system this milk bank exists. In the last three months of 2023, this place supplied one and a half tonnes of human milk to premature babies and premature babies. And last year, 2025, 4.2 tonnes of milk were delivered.”
Takeaways – Part One, Israel’s MedTech and health innovation landscape: From Tel Aviv to Jerusalem
It goes without saying that advances in artificial intelligence (AI) played a part in assisting developments within Israel during the past few years.
In this first article of the series, the importance of blood centres and whole blood donation, of rapid-response systems, of virtual reality, and general technological advancement, including robotics – all within the greater national health ecosystem setting – have been explored, specifically in terms of Israel’s recent innovations in response to national emergencies.
In Part Two, collaboration between start-ups and academia with Israel’s health ecosystem, and with industry local and abroad, will be looked at more closely and the article seek to explore how the future for life sciences looks very bright indeed.
*All images in this article are the author's own.