Spotlight on...meningitis

Sue Davie
Meningitis Trust
As part of our monthly ‘spotlight on...’ series, Sue Davie shares with us an overview on the different types of meningitis, which can affect both adults and children, and explores the treatments available for patients today. She also provides her views on how pharma can continue to help meningitis patients – by continuing to develop vaccinations.
What is meningitis?
Meningitis is inflammation of the membranes that surround and protect the brain and spinal cord. There are many different causes of meningitis, but most cases are caused by viruses and bacteria.
• Viral meningitis is usually a mild disease, but it can make people very unwell. It is estimated that many thousands of cases occur each year, mostly affecting babies and children. Although most people will make a full recovery, some are left with persistent headaches, tiredness and memory loss.
• Bacterial meningitis can be life-threatening and needs urgent medical attention. Most people who suffer from bacterial meningitis recover, but many can be left with life-long after-effects including deafness, epilepsy and learning difficulties and one in ten will die.
• Meningococcal septicaemia – meningococcal bacteria are the most common cause of bacterial meningitis in the UK. They can cause both meningitis and septicaemia, which people often have together.
Meningitis can strike quickly and kill within hours – its impact can last a lifetime. For those who survive, after-effects and complications can happen with any type of meningitis, but are more common with bacterial meningitis.
 ,
"Meningitis can strike quickly and kill within hours – its impact can last a lifetime."
 ,
Who is at risk?
Meningitis can affect anyone of any age at any time. However, there are at-risk groups:
• Babies, toddlers and young children under 5 are the most at risk group for meningitis, with around half of all cases occurring in this age group.
• Teenagers and young people, particularly first year university and college students are second most at risk from meningitis.
• Adults over 55 years are also at increased risk as the immune system weakens with age.
What are the symptoms to look out for?
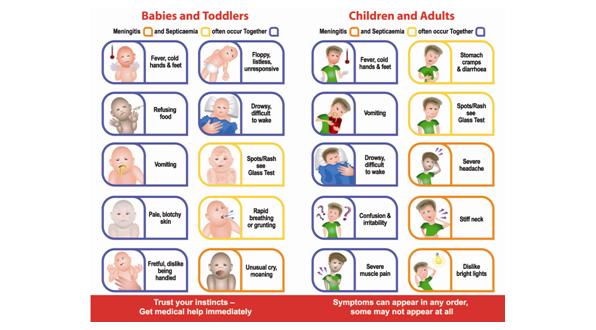
The early symptoms of meningitis such as fever, headache, nausea and muscle pain can easily be mistaken for more common illnesses such as ‘flu. It is important to know all the signs and symptoms of meningitis and septicaemia. These can appear in any order and some may not appear at all. If meningitis or septicaemia is suspected, urgent medical help is needed.
Figure 1: Meningitis symptoms checker, for babies, children and adults.
The Meningitis Trust states “do not wait for a rash to develop before seeking medical help.” Recent research carried out by the Trust showed that 71% of people immediately think of a rash when identifying meningitis. A rash can be a late sign, and in some cases it does not occur at all.
What treatment is available?
Bacterial meningitis and septicaemia require rapid admission to hospital and urgent treatment with antibiotics. If treated promptly, they are less likely to become life threatening.
Viral meningitis is rarely life threatening, but symptoms can be very similar to those of bacterial meningitis. Until bacterial meningitis has been ruled out patients may be treated with antibiotics. Once viral meningitis has been diagnosed patients can often return home, but will need plenty of rest, fluids and pain relief. There is no specific treatment for most cases of viral meningitis. An exception to this is, if herpes simplex is identified as the cause, treatment with the antiviral drug Aciclovir is possible.
 ,
"Effective vaccines are available to prevent some types of meningitis, but not all..."
 ,
One of the main investigations carried out to diagnose meningitis is a lumbar puncture. This allows a quick diagnosis of meningitis by analysing the CSF (cerebrospinal fluid) that protects the brain and spinal cord. This fluid becomes infected when a patient has meningitis. Blood tests, including PCR, are also performed and are important in ensuring the correct antibiotics are used.
Is there any way to prevent meningitis?
Vaccines are the only way to prevent meningitis. Effective vaccines are available to prevent some types of meningitis, but not all, so it is important to know the signs and symptoms of meningitis and septicaemia.
Figure 2: Vaccines are the only way to try and prevent meningitis.
However, there is still no vaccine to prevent meningococcal group B disease, which is the most common cause of bacterial meningitis in the UK. Development of an effective vaccine is now a major priority and experts believe this should be achievable in the near future.
Are there any after-effects?
Following meningitis, people can be left with many different after-effects. These can range from the obvious and easily recognisable, to hidden and hard to identify results of the disease. All after-effects can be life-changing. They include:
• Hearing loss.
• Partial or full loss of vision.
• Severe brain damage (although this is not common).
• Epilepsy / seizures.
• Septicaemia, possibly resulting in limb loss or scarring.
• Learning difficulties and behavioural problems.
• Memory problems.
• Emotional impact on individuals.
What is the future and how can pharma help?
Researchers are a step closer to developing a vaccine to protect against meningococcal group B disease (MenB), the most common cause of bacterial meningitis in the UK. A vaccine trial on adolescents in Australia, Poland and Spain, published in The Lancet Infectious Diseases, has shown that over 80% of participants developed a strong immune response to the vaccine, indicating that they would be protected from the disease.
 ,
"Researchers are a step closer to developing a vaccine to protect against meningococcal group B disease..."
 ,
Although this is a welcome step forward, meningitis is not going away and will always be with us in some form or another. Many people in the UK are living with the lifelong legacy of meningitis. Early recognition and intervention remain key in the battle to beat the disease.
Key facts:
• Most people will make a good recovery from meningitis and septicaemia.
• 10% of bacterial cases result in death.
• 15% of those who survive meningitis will be left with severe after-effects including brain damage, hearing and sight loss and where septicaemia has occurred, limb loss and scarring.
• Many more survivors will be left with invisible, but life-changing after-effects, such as memory loss, tiredness, behavioural and emotional problems, depression and long-term headaches.
• Some after-effects are short term, but many will last a lifetime.
About the author:
Sue Davie is Chief executive of the Meningitis Trust. The Meningitis Trust is a charity with support and community at its heart. It is the only support-focused organisation for people who have been, and will continue to be, affected by meningitis in the UK.
It reaches 20,000 people each year through its nurse-led helpline, home visits, family days, counselling, creative therapies, one-to-one contacts, financial grants and community support, and millions more through its life-saving awareness campaigns.
Head Office: Fern House, Bath Road, Stroud, Gloucestershire GL5 3TJ.
Tel: 01453 768000.
Email: info@meningitis-trust.org
Website: www.meningitis-trust.org
24-hour nurse-led helpline: 0808 80 10 388 helpline@meningitis-trust.org
In what ways can pharma continue to help prevent meningitis?