Opening the digital door to the NHS

The UK government recently announced plans to open a ‘digital front door’ to the NHS by giving patients greater access to remote consultations – but there are still many challenges to overcome in order to to achieve this. We asked three experts – Orbital Media CEO Peter Brady, Suffolk Primary Care chief exec Paul Brown, and GP Dr Simon Rudland – for their views on what the future holds.
How realistic is the government’s aim to increase digital health consultations in the next ten years?
Peter Brady: With the frenetic pace of technological innovation we’re seeing, I have no doubt that the aims outlined could be met. However, as with all new emerging technologies, it is important the process of implementation is actioned in the right way. Moving forward too quickly, without the right checks and balances, could have many unintended consequences.
Simon Rudland: The interesting question to ask if patients want this, and will it help to manage demand?
How can it best be achieved?
Dr Simon Rudland
Brady: I think a sensible approach would be to initially deploy small scale, regional trials that allow learnings to be collected. Ironing out the kinks before widespread deployment will be critical to minimising largescale issues later on. I think this will also help to identify how to converge various technologies within the digital health consultation process.
Rudland: One of the barriers to progress, is the difficulties that digital entrepreneurs have with integrating their platforms with GP clinical systems particularly systmone. GPs are incredibly flexible if properly incentivised. The concern at the moment is the high level of stress and strain being experienced at the primary care level. Managing change requires thinking time.
Paul Brown: The government should provide direct funding to practices to deliver online consultations. They do this already for extended non-core hours consultations.
What would be the main benefits to the NHS?
Brady: ‘No show’ for appointments currently costs the NHS £1 billion per year, with many of these down to transportation failures. Remote digital consultations can help significantly reduce this as an issue. In addition, the opportunity for patients to spend less time travelling and waiting for appointments would be very appealing
Rudland: The thought is that digital consultations would provide a way of managing demand more effectively. Certainly, this may enable parts of the primary care workforce to engage in flexible working. An example might be a young parent working from home so combining consultations with working around child care needs. This may enable the workforce to expand. To date there has been no convincing evidence that digital pathways enable patients to resolve their health needs.
How much will the NHS’ infrastructure need to change?
Brown: Data security is highly important and needs to managed accordingly. There ought to be a central strategy and guidance of how this should be managed. The IT infrastructure is constantly evolving and needs to be fit for purpose.
Rudland: There are examples of remote working already, with the private sector leading the way. Synergix Health is a good example. The HHS needs to put pressure on the clinical systems providers to be more permissive in their integration with entrepreneurs.
Do you think there needs to be a cultural shift in the NHS/healthcare in general to allow for these technologies to penetrate more?
Brady: NHS professionals are already incredibly busy and under extreme pressures. So, it will be critical to win over NHS staff by ensuring that the technology creates verified improvements and efficiencies that can be easily explained to staff, that it has good usability at its core, is as intuitive as possible and avoids lengthy training as much as possible. Healthcare professionals need to be regularly canvassed during the early implementations so that the technology can be honed and improved.
What part does AI need to play? How can it improve digital health consultations?
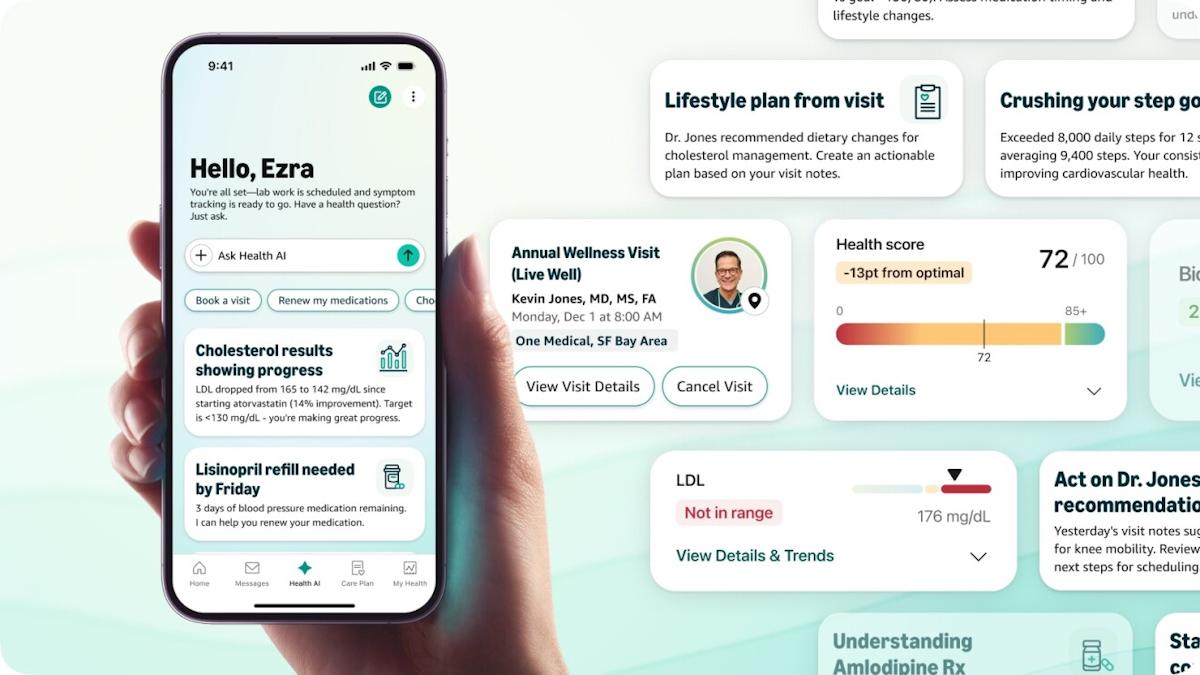
Rudland: Given a choice, would the patient want to consult with the GP, consult with an AI or consult with the GP supported by AI? I suspect the answer will be option three. The other area to consider is improving patients understanding of their illness. Using AI or augmented reality, there is a wonderful opportunity to enrich the patient’s understanding of their illness which may have compliance benefits and help to motivate lifestyle change.
What do customers and patients want to see from digital health consultations and associated apps?
Brady: Attention spans are incredibly limited within digital. So rapid facilitation of user/patient objectives is crucial. Ensuring optimal user experience and user interface design is also fundamental to patient expectations. The technology must be reliable, robust, intuitive and easy to use.
Do you often come across people who are sceptical of the idea?
Brady: Some. But broadly, the adoption of digital technologies within day to day life permeates throughout the demographic ranges. So, the development of a digital consultation access point is merely accommodating this change in user behaviour, within a healthcare context. Where we clearly have to be very careful is in ensuring that non digital savvy patients are not left behind or that quality of patient care deteriorates.
What are some of the main challenges still to overcome in implementing more digital health consultations?
Rudland: I think the biggest area that will need to be overcome is trust. There will only need to be one or two catastrophic errors for the public’s trust to be undermined.
Brown: Making an effective business case to make digital consultations worthwhile to do is difficult to do while the technology is still in development. It is clear some organisations have mastered the technology but many have not. This takes time and effort to implement at a time when clinicians workloads are already an issue remains a key challenge.
What additional tech advancements could improve digital health consultations?
Brady: One area of opportunity, which could significantly enhance the consultation experience, is the use of virtual reality. This could offer a rich, visually immersive environment for explaining and conveying complex healthcare information.
Rudland: The reach of 4G coverage and high-speed broadband is still poor particularly in remote areas where access to healthcare is difficult . These basic elements need to be a technological given.
Brown: The ability for a clinician/patient to take accurate and reliable blood pressure readings remotely would help with remote digital consultations. I believe there are emerging technologies that can do this via cameras.
About the interviewees
 Peter Brady is chief executive officer for Orbital Media. Peter is also a regular speaker at consumer healthcare events, including the Nicholas Hall International OTC Conference, AESGP and OTC ToolBox.
Peter Brady is chief executive officer for Orbital Media. Peter is also a regular speaker at consumer healthcare events, including the Nicholas Hall International OTC Conference, AESGP and OTC ToolBox.
 Dr. Simon Rudland is a GP with over 20 years of clinical experience. He is a lead partner at Stowhealth and Fellow of the Royal College of GPs and an Honorary Senior Lecturer at the University Of East Anglia.
Dr. Simon Rudland is a GP with over 20 years of clinical experience. He is a lead partner at Stowhealth and Fellow of the Royal College of GPs and an Honorary Senior Lecturer at the University Of East Anglia.
 Paul Brown is the chief executive of Suffolk Primary Care. He has been a primary care adviser to the Eastern Academic Health Science Network and previously worked as a healthcare quality improvement consultant with primary and secondary care organisations across London, the South and Eastern regions of England.
Paul Brown is the chief executive of Suffolk Primary Care. He has been a primary care adviser to the Eastern Academic Health Science Network and previously worked as a healthcare quality improvement consultant with primary and secondary care organisations across London, the South and Eastern regions of England.