Delivering innovative therapies with close industry-NHS partnerships
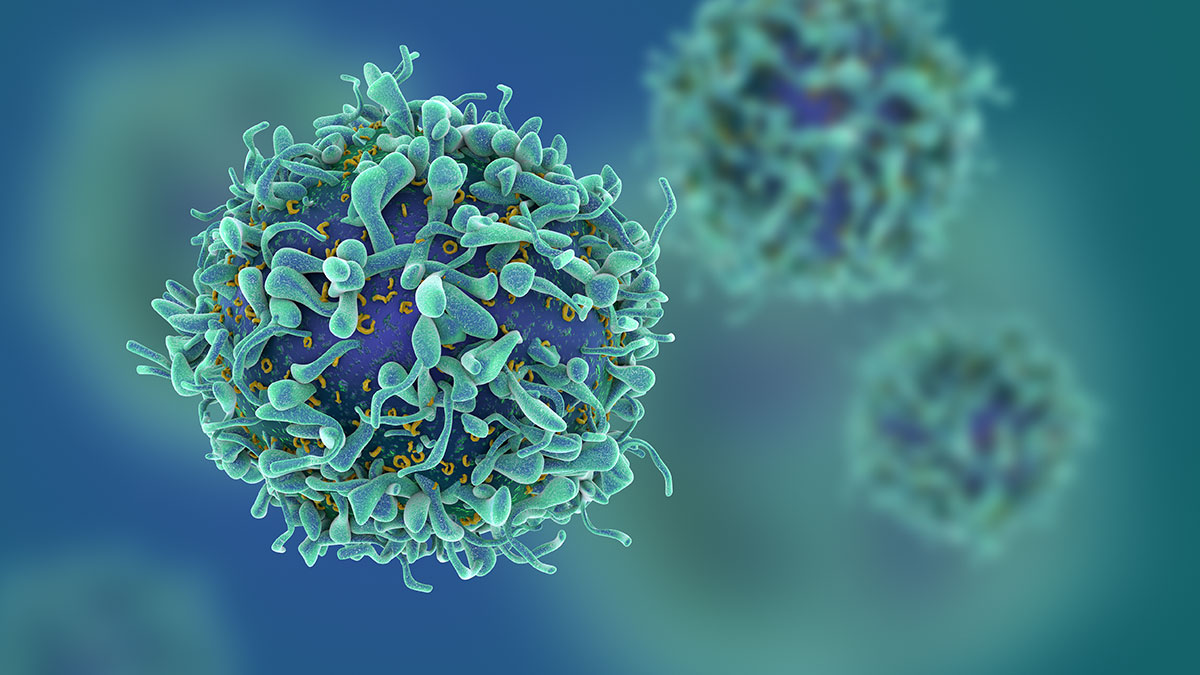
It was a crucial moment when NHS England and the National Institute for Health and Care Excellence (NICE) approved Chimeric Antigen Receptor T-cell (CAR-T) therapies for use on the NHS last year. CAR-T therapy uses a patient’s own white blood cells to fight cancer – England became one of the first countries in the world to make these innovative medicines available to patients with certain types of aggressive blood cancer.
Innovation is coming fast in cell and gene therapy, with a growing number of disease areas standing to benefit: existing CAR-T therapies are being considered for use in more conditions, and there is a broad pipeline of new products on the horizon. It is therefore important to take time to assess the way that the healthcare system approaches approving, reimbursing and using new medicines. The speed with which CAR-T was approved demonstrates that the system can be fast and flexible, but there is more to be done to make this not just the exception, but the norm.
The ambition to accelerate access to innovation has been signalled by NHS England’s chief executive, Simon Stevens, who recently announced his strategy to streamline the access arrangements for certain cancer therapies, ensuring all patients can receive the therapies they need. For me, this raises several considerations; is our medicines appraisal process fit for the future? What does great partnership between NHS and industry look like? How does this incentivise innovation in the future?
First, we need to make sure that our current system is always fit to assess this type of innovation.
Affordability calculations must consider the difference between the high initial cost of getting the system set up to deliver them against their cost further down the line. These therapies are also an entirely different proposition to mass-produced pills. As such, manufacturing a treatment tailored to each patient places constraints on the extent to which companies can flex pricing to meet NICE’s Quality Adjusted Life Year (QALY) thresholds.
In valuing the human and economic impact of personalised medicine, the system needs to begin to find the balance between affordability for the NHS and access to innovative medicines some of which could literally be life-saving. If the price is too high, it will be unjustifiable for the NHS to pay for. If too low, however, pharmaceutical companies will have limited ability to continue their substantial investments in these fields.
It is also important to capture the voices of patients and clinicians in this context, so that the most important perspectives and lived experiences can be included in deliberations. The ongoing review into NICE’s methods for medicines appraisals is certainly the right moment to address the patient and physician representation in appraisals of personalised medicines.
What about collaboration? CAR-T is only available now because the processes involved in bringing innovative medicines to patients were streamlined, with NICE and NHS England working with industry to ensure that patients could access these potentially life-saving treatments as early as possible. Now, only half a year on, the first patients with rare and aggressive forms of blood cancer have undergone treatment with licensed CAR-T products on the NHS.
It is important that we recognise the value of this partnership and build on this success to ensure there is certainty that these processes will be equally rapid for the new generation of Advanced Therapy Medicinal Products (ATMPs). In order to create a health and social care sector for the future, one that addresses the economic and scientific challenges of medicines development, it will require long-term thinking and future-focused collaboration.
As a sector, we have begun to recognise this. The NHS Long Term Plan presents an opportunity for industry to engage with the NHS regarding the direction of the health service over the next ten years.
We want UK patients to be the first to benefit from the next wave of innovative and curative treatments, which in turn allows the UK economy to draw additional investment from the life sciences sector. We can achieve this together with systematic collaboration. Earlier and regular dialogue between senior NHS policymakers and industry representatives can help to develop long-term solutions. Solutions that can support a 21st century health service, with innovation at its heart.
Recent statistics from the Office for Life Sciences found that while the UK is among the best global performers for research and development, it takes far longer to actually adopt and use new medicines than in many other countries. However as seen with CAR-T, the NHS is engaging with industry in a way that it has not done previously. As an industry we must continue to find constructive ways to collaborate with the NHS, on issues such as innovation, access and a more flexible commercial environment. The Life Sciences Industrial Strategy and the subsequent Sector Deals have also shown that government and industry can have serious and effective discussions about the future of the sector.
There is much to be excited about in the life sciences at present. The advances in understanding diseases and developing targeted, personalised therapies offers real hope to patients who otherwise might not survive. Our scientists, our industry and our NHS all have the same ambition to help people live longer, healthier lives than ever before and, by working together, this ambition will be achieved.
About the author
 Hilary Hutton-Squire is vice president and general manager of Gilead Sciences in the UK and Ireland. Hilary has 20 years of extensive industry experience, with 15 years in leadership roles with both in-country and international scope, including previous roles at Novartis, IMS Health and GSK. Hilary’s wide experience includes working in oncology, antivirals, inflammation, respiratory, ophthalmology and rare genetic diseases.
Hilary Hutton-Squire is vice president and general manager of Gilead Sciences in the UK and Ireland. Hilary has 20 years of extensive industry experience, with 15 years in leadership roles with both in-country and international scope, including previous roles at Novartis, IMS Health and GSK. Hilary’s wide experience includes working in oncology, antivirals, inflammation, respiratory, ophthalmology and rare genetic diseases.











