Organoids: bringing life to precision medicine
Swiss-based biotech QGel is hoping to offer a novel approach to precision medicine by solving several of the current challenges with ‘organoids’, which can be used to test medicines on organ-like tissue cultures. Founder and CEO Dr Colin Sanctuary tells us more.
The vital job of precision medicine is to match the right drugs to the right patients. In cancer precision medicine, this generally means to identify the treatment that will best decrease the tumor size or even eradicate the patient’s cancer.
But there are still critics that put the entire concept of precision medicine into question. My view is that Next-Generation Genetic Sequencing (NGS) for precision medicine, as fantastic as it is, still largely relies on collecting huge amounts of somewhat abstract genetic data on the patient. In theory, a specific treatment is identified by computationally comparing “big data” to a reliable set of even “bigger data” with the hope of finding the right treatment. In practice, this approach shows that only 7% of cancer patients benefit from this genomic approach to precision medicine.
So when I think about the shortfalls in precision medicine, it really comes down to data. Too much of precision medicine relies on ambiguous big data. We need to improve the data we get from the patient and I like to call this improved data “smart data”. By smart data I mean acquiring small sets of highly accurate data that enhance the big data that make it more usable. Testing cancer therapies on living patient cancer cells, or organoids, is an example of an approach to generate smart data that offers tremendous promise.
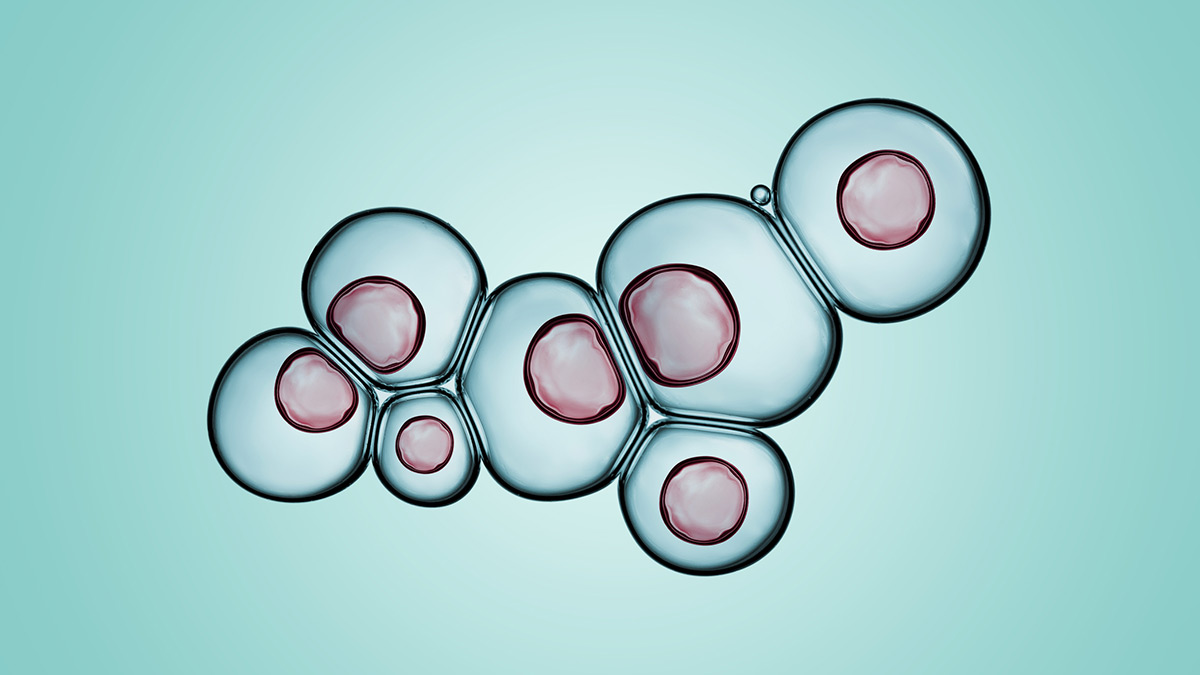
Organoids are derived from living cells taken from a patient that are grown outside of the patient in a way that very closely mimics the unique biological features of that patient’s tissue. This ability to grow ‘mini-patient tumour avatars’ in vitro offers a unique opportunity to test a vast array of potential drugs on the patient’s cancer cells to observe how those cells will react to each treatment option, before treating the patient.
Organoid publications in top journals indicate that this functional approach can successfully match the right drug to a specific patient almost 90% of the time, and event predict which drug would not work 100% of the time.
Growing organoids
To grow organoids, you need three key ingredients: the patient cells, a gel, and the media (a type of food for the cells). QGel’s core and proprietary technology relates to the gel.
Looking at the gel more closely, the human body is made up of more than 200 different types of cells. Surrounding these cells is gel, aka an extracellular matrix (ECM), a gooey, complex network of biological, biophysical and biochemical components that regulates tissue behaviour. Changes in the conditions of the ECM (growth factors, cytokines, aberrant proteases, hormones, tissue architecture, etc.) affect tissue homeostasis, and can lead to the onset of diseases such as cancer. More simply said, you need a gel to grow organoids.
Organoids need a ‘host’ ECM located outside of the patient’s body, in which those patient’s cancer cells can be embedded and continue to grow as though they were still in the patient’s body. The most commonly used gel used today for organoids is an animal-based gel derived from cancer-induced in mice. The animal-gel extracted from these mice provides the structural features as well as a vast amount of unidentified proteins that enable organoids formation. The problem, in addition to ethical and batch-to-batch quality concerns, is that these animal-based gels are undefined in composition, making them very difficult to scale. Not being able to scale is not such a problem for basic scientific research where very few samples are used but using animal-gels for clinical decision making is entirely unsuitable.
We overcome this limitation by designing fully synthetic ECMs, which like the animal-based alternative, allow for the biologically accurate 3D growth of any human tissue, diseased or healthy, outside of the human body. Unlike the animal-based alternative, however, this provides a fully defined synthetic composition, where all the elements of the gel are known and is thus able to be manufactured in large quantities with no batch-to-batch variation.
Challenges
The challenge is that the functional approach of organoids requires that the cancer biopsy sample under study be fresh, a handling protocol that is not currently a part of standard clinical workflows. On top of this, growing organoids requires specialised skills, materials and methods that are perceived as cumbersome, time-consuming, labour-intensive and expensive.
So, in my opinion, the best way to make precision medicine help as many patients as possible is to bring functional tests to patients and make smart data accessible to all patients. To do this we need to use efficient and cost-effective methods to standardise organoids so that smart data benefits patients. This smart data will complement existing sets of NGS data, which in turn will improve the predictive power of computational methods for better patient treatment.
At QGel we have figured out how to standardise organoids. Having scaled these functional tests successfully today we are working to roll this out into a clinical workflow to treat at first a few hundred patients per year to, one day perhaps thousands of patients per day. For the time being, our focus has been on cancer but one could imagine many other potential areas of development.
Clinical challenges aside, there are other forces that start to come into play to make precision medicine a reality for patients.
First is about the payors. Who will pay for such a novel test? Funding bodies, health ministries and insurance companies stand to benefit significantly from precision medicine, and they will need to get involved to properly assess the economic benefit of this novel approach. Payors should get involved early on – even fund precision medicine studies – to identify areas where certain interventions would reduce the cost of the disease as well as to reduce suffering. When payors are equipped with the information to communicate which therapies are adequate for a patient, and which ones are not adequate, the revolution in saving on healthcare costs will begin.
Second, the dynamics of how treatments are reimbursed must change when precision medicine emerges as a cost-saving tool. Instead of limiting which treatments are paid for, which is the case today, payors should devise a scheme that shifts the cost of prescribing ineffective drugs, to offering an incentive to prescribe and reimburse predictive diagnostic screening tests. Ultimately, this would be in the best interest of the most important stakeholder: the patient.
Third, physicians will need to be informed about new precision medicine tools and understand how to integrate them into their clinical workflows. They will also need to trust the data and conclusions drawn from them, which would require regulations to ensure data quality and patient-data privacy. Precision medicine modules would need to enter the curriculum of medical schools and technical staff would need to be trained on point-of-care protocols.
Fourth, patients will need to be informed early on and be encouraged to share their health data and be reassured on data privacy. Sharing medical data is at the crux of precision medicine and measures will need to be taken at the government level to encourage this.
Organoids are not science fiction, the science is very real but they are not yet practical for routine clinical practice to directly benefit patients cost-effectively. I believe the last remaining technical barrier is to replace the animal-based gels with a fully defined synthetic alternative. At QGel we have achieved this, and now we look forward to demonstrating this in a regulated setting to make this technology accessible to more patients.












