A history of the pharmaceutical industry

The 21st century pharmaceutical and biotech sector has come a long way from its roots in 19th century pharmacy. pharmaphorum looks at its evolution over the centuries.
The roots of the pharmaceutical industry lie back with the apothecaries and pharmacies that offered traditional remedies as far back as the middle ages, offering a hit-and-miss range of treatments based on centuries of folk knowledge.
But the industry as we understand it today really has its origins in the second half of the 19th century. Whilst the scientific revolution of the 17th century had spread ideas of rationalism and experimentation, and the industrial revolution had transformed the production of goods in the late 18th century, the marrying of the two concepts for the benefit of human health was a comparatively late development.
Merck in Germany was possibly the earliest company to move in this direction. Originating as a pharmacy founded in Darmstadt in 1668, it was in 1827 that Heinrich Emanuel Merck began the transition towards an industrial and scientific concern, by manufacturing and selling alkaloids.
Similarly, whilst GlaxoSmithKline’s origins can be traced back as far as 1715, it was only in the middle of the 19th century that Beecham became involved in the industrial production of medicine, producing patented medicine from 1842, and the world’s first factory for producing only medicines in 1859.
America's pharmaceutical founding fathers
Meanwhile in the USA, Pfizer was founded in 1849 by two German immigrants, initially as a fine chemicals business. Their business expanded rapidly during the American civil war as demand for painkillers and antiseptics rocketed.
Whilst Pfizer was providing the medicines needed for the Union war effort, a young cavalry commander named Colonel Eli Lilly was serving in their army. A trained pharmaceutical chemist, Lilly was an archetype of the dynamic and multi-talented 19th century American industrialist, who after his military career, and trying his hand at farming, set up a pharmaceutical business in 1876. He was a pioneer of new methods in the industry, being one of the first to focus on R&D as well as manufacturing.
Another military man in the drugs business was Edward Robinson Squibb, who as a naval doctor during the Mexican-American war of 1846–1848 threw the drugs he was supplied with overboard due to their low quality. He set up a laboratory in 1858, like Pfizer supplying Union armies in the civil war, and laying the basis for today’s BMS.
"Whilst Pfizer was providing the medicines needed for the Union war effort, a young cavalry commander named Colonel Eli Lilly was serving in their army"
Switzerland also rapidly developed a home-grown pharmaceutical industry in the second half of the 19th century. Previously a centre of the trade in textiles and dyes, Swiss manufacturers gradually began to realise their dyestuffs had antiseptic and other properties and began to market them as pharmaceuticals, in contrast to the origin in pharmacies of other enterprises. Switzerland’s total lack of patent laws led to it being accused of being a “pirate state” in the German Reichstag. Sandoz, CIBA-Geigy, Roche and the Basel hub of the pharmaceutical industry all have their roots in this boom.
1900s - Aspirin arrives
It wasn’t just Swiss companies that had their roots in the dye trade. Bayer was founded in 1863 as a dye maker in Wuppertal, the hometown of Karl Marx’s collaborator Friedrich Engels. It later moved into medicines, commercialising aspirin around the turn of the 20th century, one of the most successful pharmaceuticals ever at that point.
The unregulated nature of the trade in medicines during this period ensured there was a far less strict delineation between 'pharmaceutical' and 'chemical' industries than we have nowadays. These companies focused as much on cod liver oil, toothpaste, citric acid for soft drinks, and hair gel as on prescription medicines, as well as selling products like heroin on the over-the-counter market.
The national rivalries and conflicts that characterised this period also had their impact on the developing industry.
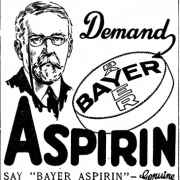
An advert for Bayer's Aspirin from the early 20th century
Bayer had the aspirin trademark and its US assets seized during World War One, whilst “American” Merck (now Merck & Co. in the US or Merck Sharp & Dohme (MSD) elsewhere) was compulsorily split off from its Germany parent company (Merck KGaA) at the same time. Bayer also had its Russian subsidiary seized during the Russian revolution. This disruption to Germany’s position as the leader in pharmaceuticals in the early 20th century by the war meant that others, particularly in the US, could take relative advantage. The beginnings of the globalisation of the industry were seen both before and after the war – in the UK, import duties incentivised many foreign companies such as Wyeth, Sandoz, CIBA, Eli Lilly and MSD to set up subsidiaries in Britain in the post-war years.
The interwar years
The period between 1918 and 1939 was marked by two breakthroughs that presaged the arrival of the pharma industry as we know it today. The first was insulin – Frederick Banting and colleagues managed to isolate insulin that could treat diabetes, up until that point a fatal condition. But it was only in collaboration with the scientists at Eli Lilly that they were able to sufficiently purify the extract and industrially produce and distribute it as an effective medicine.
The second was penicillin, a discovery of an impact possibly unparalleled by any other in medicine. After Alexander Fleming’s initial discovery of the penicillium mould’s antibiotic properties in 1928, and Howard Florey and Ernst Chain’s further experimentation, a government-supported international collaboration including Merck, Pfizer and Squibb worked on mass producing the drug during World War Two, saving thousands of soldiers’ lives. The immense scale and sophistication of the penicillin development effort marked a new era for the way the pharmaceutical industry developed drugs. The war had also encouraged research into everything from new analgesics to drugs against typhus, with a great deal of collaboration between the companies and government.
Post-war period
After the war, the arrival of social healthcare systems such as the UK’s National Health Service (NHS) in Europe created a much more structured system, both for prescription of drugs and their reimbursement. In 1957, the NHS brought in what was essentially a price fixing scheme to allow reasonable return on investment for drug manufacturers, solidifying the incentive to invest in new medicines.
The US pharmaceutical industry was booming, thanks to being part of the world's biggest and most dynamic economy. Its growth was also helped by generous funding from the government, with the National Institutes of Health seeing its federal funding rise to nearly $100 million by 1956. This investment fuelled the development of drugs to come over the coming decades.
Meanwhile, as the industry grew wealthy thanks to its growing portfolio of products, the potential ethical conflicts of making money from selling healthcare products became increasingly apparent.
George Merck addressed this question directly in 1950, proclaiming that: "We try never to forget that medicine is for the people. It is not for the profits. The profits follow, and if we have remembered that, they have never failed to appear. The better we remember it, the larger they have been."
This public-spirited industry still required greater oversight, however, and government regulations on medicines increased on both sides of the Atlantic.

George Merck on the cover of Time magazine
Thalidomide and the development of drug safety regulation and monitoring
The Thalidomide scandal of 1961 prompted an increase in the regulation and testing of drugs before licensing, with a new amendment to US Food and Drug Administration (FDA) rules demanding proof of efficacy and accurate disclosure of side-effects for new medications (the Kefauver-Harris Amendment) being implemented in 1962. Likewise, the 1964 Declaration of Helsinki put greater ethical structures on clinical research, clearly cementing the difference between production of scientific prescription medicines and other chemicals.

The FDA's Frances O Kelsey: by blocking approval of Thalidomide in the US, Kelsey prevented thousands of children being born with life-changing deformities. Photo: FDA
Fordian methods enabled more rational methods of mass production, and increasing understanding of biology and chemistry enabled drug candidates to be chosen systematically rather than discovered serendipitously. This ‘golden age’ of drug development took place in the broader landscape of the post-war boom, a general context of massive improvements in standards of living and technological optimism that characterised the 40s to the early 70s, as well as the science-boosting competition of the cold war. As the barriers to entry in drug production were raised, a great deal of consolidation occurred in the industry. Likewise, the processes of internationalisation begun before the war were continued – in 1951 alone Pfizer opened subsidiaries in nine new countries.
The list of novel drugs from the post-war era speaks for itself. The contraceptive pill, introduced in 1960, had an impact on society almost as massive as that of penicillin, enabling women to effectively control their fertility and enabling sexual equality for the first time. Valium (diazepam) was brought to the market by Roche in 1963, followed by the introduction of the monoamine oxidase inhibitor (MAOI) class of anti-depressants and antipsychotic haloperidol.
These drugs ushered in a new era of psychiatric treatment, adding pill-based treatments to the psychoanalytic ones that had previously characterised psychiatry in this era. The 1970s provided a wave of cancer drugs, as part of the US government’s “war on cancer”, a recent report from Cancer Research UK showed that survival rates have doubled since the early 70s – due in large part to the massive innovation in oncology medicines that has occurred since then. ACE inhibitors arrived in 1975, improving cardiac health, and even drugs as ubiquitous as paracetamol and ibuprofen were developed in 1956 and 1969 respectively.
As the 1970s drew to an end, a shift began in the way the pharma industry focused its energies. In 1977, Tagamet, an ulcer medication, became the first ever “blockbuster” drug, earning its manufacturers more than $1 billion a year and its creators the Nobel Prize. This marked a new departure as companies competed to be the developer of the next big blockbuster, and many achieved great success. Eli Lilly released the first selective serotonin reuptake inhibitor (SSRI), Prozac, in 1987, once again revolutionising mental health practice. The first statin was also approved in 1987, manufactured by Merck (MSD).
New challenges in an age of innovation
The 2010s have seen the development of innovative new classes of medicines, building on the greater understanding of the body since the genome was first sequenced at the end of the last century.
This knowledge of genetics and the underlying cause of many diseases, including cancer, has resulted in powerful new drugs.
In cancer, the pharma industry has begun producing immunotherapies, which do not act directly against the disease but instead enlist the immune system to fight against malignant tissues.
The idea of immunotherapy had been around since the late 1900s, but it was companies such as Bristol-Myers Squibb and its CTLA4 class melanoma drug Yervoy (ipilimumab) that began the revolution.
This was followed by Merck & Co’s Keytruda (pembrolizumab) and a gang of rival PD-L/PD-L1 checkpoint inhibitors, which have set new standards in cancer care in many different forms of the disease.
The importance of cancer immunotherapy was underlined in 2018, when James Allison and Tasuku Honjo were granted the Nobel Prize for their early work on CTLA4 and PD-1 checkpoint inhibitors, respectively.
With CAR-T (chimeric antigen receptor T-cell) drugs, pharma companies have taken the idea one step further and have been able to genetically modify the patient’s own cells to fight cancer.
This deep knowledge of genetics has also led to the development of the first ever gene therapies, and there are now treatments capable of addressing the underlying causes of certain rare diseases with a single shot.
This, along with other innovations such as antisense technology, has led to drugs for rare diseases that were previously considered untreatable.
Meanwhile, in infectious diseases, the pharma industry has been able to produce effective drugs that could lead to the eradication of hepatitis C in the next few years.
And in 2020 the pharma industry produced dozens of potential vaccines for the COVID-19 pandemic in record time, as the world fights the new and deadly coronavirus pandemic.
But there are challenges: the new generation of drugs are expensive and have pushed the limits of health care systems’ finances as well as the boundaries of science.
With its hepatitis C drugs, Gilead faced huge amounts of controversy over the initial costs of its therapies, although these were reduced drastically over time as more competitors came to market.
And firms such as Vertex have added to the controversy with tough pricing demands for new therapies for cystic fibrosis, leading to stand-offs lasting several years with payers in countries such as the UK.
While the industry has made huge achievements in some areas, research into new antibiotics has stagnated as they do not create the revenues big pharma companies are looking for – and this comes at a time when the world is still coming to grips with the scale of the threat from antimicrobial resistance.
The future is bright for the pharma industry, but maintaining public trust and preventing millions of deaths from antibiotic resistant bacterial strains are two major challenges it must overcome as the century progresses.











