Expanding the haematology toolkit: Insights and operational imperatives from ASH 2025

The 2025 American Society of Hematology (ASH) meeting in December presented a clear message: scientific innovation and stakeholder collaboration are driving haematology forwards even as regulatory and access challenges demand fresh solutions. Outgoing ASH President Dr Belinda Avalos issued a powerful call to “fight for science, fight for research, fight for haematology, and fight for our patients.”
With more than 8,200 abstracts accepted, ASH 2025 showcased breakthroughs in sickle cell disease, platelet disorders, and next-generation cell therapies, alongside operational strategies for expanded clinical trial access. From repurposed drugs and novel mechanisms to agile treatment paradigms and off-the-shelf cellular approaches, discussions and presentations underscored a future focused on reducing toxicity, improving quality of life and embedding equitable access into trial design to ensure that progress translates into meaningful impact for patients worldwide.
Reimagining sickle cell disease care: From successful drug repurposing to novel mechanisms
Sickle cell disease (SCD) presentations at ASH 2025 reflected a broader commitment to addressing the complex pathophysiology of SCD through repurposed therapies, novel mechanisms, and tailoring operational strategies to improve global access.
Several presentations underscored a growing interest in moving beyond traditional haemoglobin-centric approaches to drug repurposing and therapeutic diversification for SCD. Hydroxyurea (HU) remains the cornerstone for inducing foetal haemoglobin (HbF), but challenges with patient adherence due to frequent blood monitoring and dosing adjustments leave a critical gap in care. To address this, a Phase I study evaluated panobinostat, an oral histone deacetylase inhibitor originally developed for oncology, in patients with severe SCD who were intolerant of HU therapy. Early findings demonstrated that panobinostat was generally well tolerated, with manageable gastrointestinal symptoms and mild cytopenias, while several participants achieved clinically meaningful increases in HbF. These results suggest panobinostat may offer an alternative for high-risk patients and warrants further investigation into dosing strategies and long-term outcomes.
Expansion of existing SCD treatments into a paediatric population was also touted at ASH. Preliminary data from the CLIMB SCD-151 Phase III study on the safety and efficacy of gene-editing therapy exagamglogene autotemcel in children as young as five years old with severe SCD was presented. As of the latest follow-up, all paediatric participants remained free of vaso-occlusive crises for up to two years after receiving the one-time therapy. This success supports planned regulatory expansion in paediatric use.
Complementing this, the ACHiEvE-SCD trial explored the addition of exogenous erythropoietin to HU in patients with persistent anaemia. The combination improved haemoglobin levels and quality-of-life measures across multiple domains without introducing unexpected safety concerns. This emphasises how optimising existing regimens can deliver meaningful benefits for patients who remain symptomatic despite standard therapy.
Beyond repurposing, researchers at ASH highlighted novel mechanisms of action aimed at inflammation, vascular health, and lipid metabolism. A Phase II open-label study of epeleuton, a potential novel therapy that targets two important aspects of SCD — red blood cells and inflammation of blood vessels — found improvement in red blood cell membrane integrity, as well as reduced haemolysis, inflammation, endothelial adhesion, and organ damage in patients with SCD. Also, certain agents, such as rilzabrutinib (a Bruton tyrosine kinase or BTK inhibitor), shown to target inflammatory pathways in pre-clinical SCD models and clinically in ITP and warm autoimmune haemolytic anaemia, signal a shift toward multi-pronged approaches that address the complex pathophysiology of SCD. A Phase III clinical trial in SCD is planned. These outcomes reflect a growing recognition that haemoglobin-centric strategies alone may not fully mitigate disease burden.
Operationally, global representation and trial access continues to be top-of-mind for the community, with multiple trial outcomes from Uganda discussed at the meeting reinforcing the need for culturally sensitive trial design and infrastructure for equitable access. ASH’s special interest sessions on international outreach echoed this priority, emphasising partnerships with local investigators and community-based haematologists in the Middle East and North Africa to overcome barriers in underserved regions. For example, in another special interest session focused on the importance of clinical trials and enrolment reflecting disease epidemiology, Jeffrey Keefer, head of IQVIA’s Therapeutic Science and Strategy Unit, emphasised the role of clinical research organisations in embedding critical representation principles into trial design, particularly rare disease trials and reaching community-based haematologists to gauge nuanced challenges.
Platelet disorders: From episodic rescue toward disease modification
Conference participants also showed strong interest in immune thrombocytopenia (ITP) management and the promise of emerging therapies with disease-modifying potential, rather than transient platelet elevation through existing first-line therapies (e.g., corticosteroids). One notable abstract was the VAYHIT2 Phase III study, which evaluated ianalumab, an anti-B-cell activating factor receptor monoclonal antibody, in adults with early ITP who relapsed after steroids. All patients received eltrombopag, an oral thrombopoietin receptor agonist, plus ianalumab (3 mg/kg or 9 mg/kg) or placebo.
Both doses of ianalumab significantly extended time-to-treatment failure, with a median of 13 months compared to 4.7 months for placebo. At six months, stable platelet response was achieved in 62% (9 mg/kg) and 56.9% (3 mg/kg) compared to 39.2% in controls. Also, overall, fatigue scores improved without increased infection risk despite B-cell depletion. These collective findings suggest ianalumab offers a disease-modifying profile, enabling durable remission with a predefined duration of therapy, rather than short-term platelet boosts. Given the response in an early disease stage, these outcomes may position ianalumab as a second-line therapy option, emphasising moving up disease-modifying strategies in the treatment course.
Similarly, the PROLONG programme explored strategies to optimise anti-CD20 therapy for ITP through anti-CD20 monoclonal antibody rituximab induction with or without dexamethasone and maintenance with low-dose rituximab. The two-phase study evaluated whether there is potential for sustained disease remission, rather than episodic rescue.
The induction phase found that adding a moderate dose dexamethasone to rituximab substantially improved the initial response compared to rituximab alone, with 37.5% of patients achieving a response at week 24 to rituximab alone versus 60.3% in the combination arm and delayed the time to first bleeding. Additionally, early insights indicate that maintenance rituximab prolonged response duration, reinforcing a broader trend toward proactive, long-term management, rather than short-term platelet boosts. Adopting these disease-modifying strategies will require updates to the drug development infrastructure, including:
- Streamlined transitions from steroids to second-line therapy.
- Pragmatic trial designs incorporating quality-of-life endpoints.
- Monitoring and patient education to support induction-maintenance models.
- Ongoing payer engagement on durability and steroid-sparing benefits.
Ongoing mission: From minimising toxicity and burdens to broadening access
The global haematology community continues to push for ways to broaden access to effective therapies while reducing toxicity and logistical burdens that can hinder real-world use.
Challenging the status quo
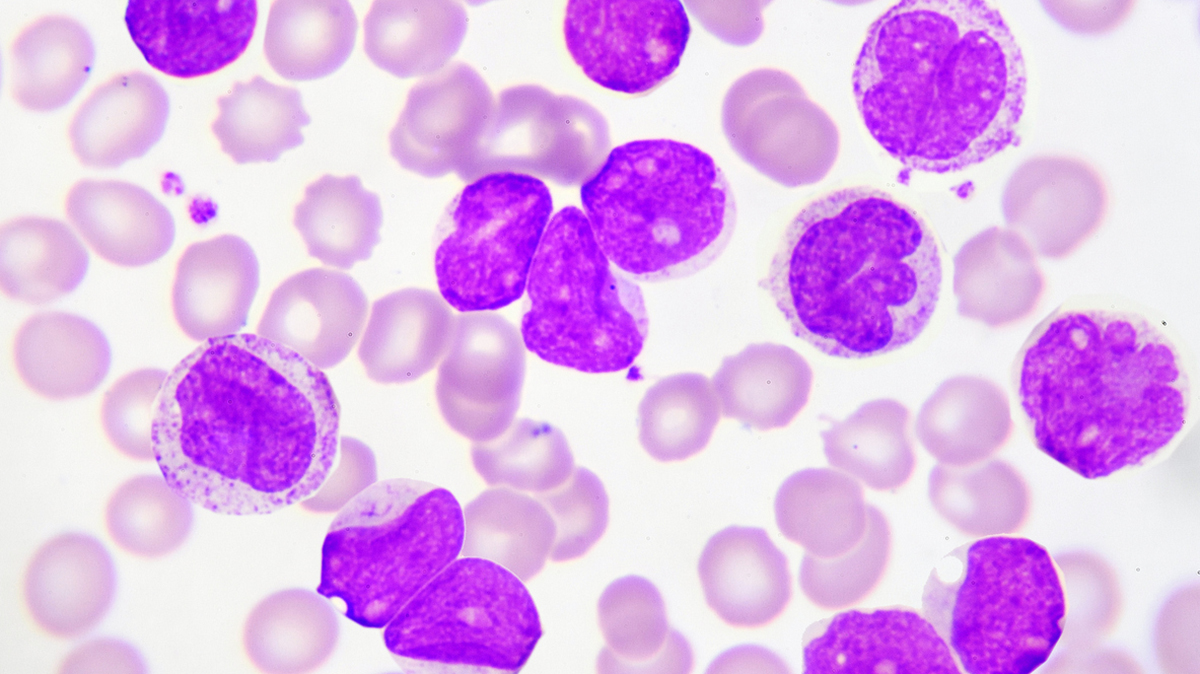
For decades, intensive chemotherapy, relying typically on cytarabine plus an anthracycline (“7+3”), has been the standard first-line treatment for fit patients with acute myeloid leukaemia. However, this approach is associated with significant toxicity, prolonged hospitalisation, and poor long-term outcomes.
Data presented at ASH suggests that the combination therapy of the hypomethylating agent azacitidine and the BCL 2 inhibitor venetoclax, historically reserved for older or unfit patients, may offer comparable efficacy in fit individuals. In this Phase II study, this combination therapy achieved high complete remission rates, noteworthy minimal residual disease negativity, and lower early mortality, while also reducing toxicity and in-patient burden compared to standard intensive chemotherapy.
For fit patients with AML, these findings challenge the long-standing paradigm requiring aggressive chemotherapy to attain good responses. If these outcomes are further supported in Phase III studies, this combination therapy could decrease the patient burden while maintaining benefit.
Preclinical data on PRT12396, a highly selective inhibitor targeting the JAK2V617F mutation found in myeloproliferative neoplasms also met the theme of decreasing toxicity while maintaining good outcomes. Aiming to spare wild-type janus kinase 2 (JAK2) function to reduce haematologic toxicities commonly associated with current JAK inhibitors, PRT12396 demonstrated potent inhibition of mutant JAK2 signaling, normalisation of blood counts, and reversal of disease features without significant off-target effects. The compound showed a favourable safety profile in early toxicology studies, supporting its potential as a next-generation therapy for patients with myeloproliferative neoplasms. The developer anticipates filing an Investigational New Drug submission in early 2026.
CAR-T therapies: Impact of off-the-shelf and autoimmune applications
ASH 2025 featured promising data on base-edited allogeneic chimeric antigen receptor 7 T-cell therapies (CAR7-T cells) for relapsed/refractory paediatric T-cell acute lymphoblastic leukaemia (T-ALL). These donor-derived cells, engineered to target CD7, demonstrated robust CAR-T cell expansion (>100-fold) and persistence for up to three months with no late-onset serious adverse events. Several patients successfully bridged to allogeneic haematopoietic stem cell transplantation and maintained remission from three to 36 months post-transplant.
With positive outcomes, this approach can help tackle the logistical hurdles of autologous CAR-T manufacturing and uses base editing to minimise graft-versus-host disease risk, paving the way for more accessible CAR-T in T-ALL for this vulnerable patient population.
The CARLYSLE Phase I trial evaluated obecabtagene autoleucel, a CD19-targeting CAR-T therapy, in severe refractory systemic lupus erythematosus (SLE). Among nine patients, no dose-limiting toxicities or immune effector cell-associated neurotoxicity syndrome occurred at the 50 × 10⁶ dose. Cytokine release syndrome was mostly Grade 1 or 2 and manageable. At this dose, 50% of patients achieved complete renal response and 83% reached definition of remission in SLE by five months, sustained through one year. Profound B-cell depletion and transient CAR-T persistence (approximately three months) were seen as expected. These findings support expansion into lupus nephritis in the upcoming LUMINA Phase II study.
These approaches may help overcome logistical challenges of autologous CAR-T and expand applications into autoimmunity. As such, they will also require clinical trial sponsors and CROs to plan and design new operational workflows and intricate cross-specialty coordination from end-to-end.
From breakthroughs to real-world change: What’s next for haematology?
ASH 2025 closed on a note of optimism and urgency: science is advancing rapidly, but translating breakthroughs into real-world impact for patients worldwide requires continued collaboration and underscores the need for innovation not only in treatment, but in trial design and delivery.
From repurposed agents and novel mechanisms in classical haematology to next-generation cell therapies and operational strategies for global trial access, the meeting highlighted a future defined by precision, durability, and access. As stakeholders unite under the banner of advocacy and progress, haematology’s momentum promises meaningful change for patients worldwide.
About the authors
 Michael Armstrong, MD, PhD, is senior director, medical, at the Hematology-Oncology Center of Excellence at IQVIA Biotech. He is a paediatric haematologist-oncologist with a special interest in basic science and translational research in haematologic malignancies. He works closely with biotech companies to assist with new drug development and the administration of clinical trials, with an emphasis on immuno-oncology and paediatric indications. In his previous work with the world’s largest paediatric cancer research group, the Children’s Oncology Group, Armstrong participated in the neuroblastoma section, including the biology subcommittee and a trial study committee.
Michael Armstrong, MD, PhD, is senior director, medical, at the Hematology-Oncology Center of Excellence at IQVIA Biotech. He is a paediatric haematologist-oncologist with a special interest in basic science and translational research in haematologic malignancies. He works closely with biotech companies to assist with new drug development and the administration of clinical trials, with an emphasis on immuno-oncology and paediatric indications. In his previous work with the world’s largest paediatric cancer research group, the Children’s Oncology Group, Armstrong participated in the neuroblastoma section, including the biology subcommittee and a trial study committee.
 James French, MD, is senior medical director at the Hematology-Oncology Center of Excellence at IQVIA Biotech and medical strategy lead, haematology, at IQVIA. As a board-certified paediatric haematologist-oncologist with a special interest in classical haematology, particularly bleeding disorders and haemoglobinopathies, French works closely with large and mid-size pharma and biotech companies to plan and initiate haematology clinical trials for developing new drugs and biologics in Phase I through IV settings for adults and paediatrics. Prior to IQVIA, French spent 24 years in clinical practice as medical director at haemophilia treatment centres, associate medical director of comprehensive sickle cell centres, and principal investigator in multiple haematology and oncology trials.
James French, MD, is senior medical director at the Hematology-Oncology Center of Excellence at IQVIA Biotech and medical strategy lead, haematology, at IQVIA. As a board-certified paediatric haematologist-oncologist with a special interest in classical haematology, particularly bleeding disorders and haemoglobinopathies, French works closely with large and mid-size pharma and biotech companies to plan and initiate haematology clinical trials for developing new drugs and biologics in Phase I through IV settings for adults and paediatrics. Prior to IQVIA, French spent 24 years in clinical practice as medical director at haemophilia treatment centres, associate medical director of comprehensive sickle cell centres, and principal investigator in multiple haematology and oncology trials.
 Sarah Kromrey, PhD, is senior director of therapeutic strategy at IQVIA Biotech. Specialising in rare haematologic diseases, Kromrey partners with biotech companies and cross-functional teams to shape strategic clinical trial planning and execution, with a focus on accelerating access to innovative treatments for patients.
Sarah Kromrey, PhD, is senior director of therapeutic strategy at IQVIA Biotech. Specialising in rare haematologic diseases, Kromrey partners with biotech companies and cross-functional teams to shape strategic clinical trial planning and execution, with a focus on accelerating access to innovative treatments for patients.