Economist Impact: World Cancer Series – pharmaphorum in attendance, day one (part iv)
To conclude pharmaphorum’s look back at day one of The Economist’s 8th Annual World Cancer Series congress in Brussels, Belgium, in November – where the foci were “innovation, equity, and excellence” - after the panel, ‘The future of European cancer control in a time of crisis’, came The Economist’s health policy editor Natasha Loder’s interview with Dame Kate Bingham, managing partner at SV Health Investors and former chair of the UK Government’s Vaccine Taskforce during the pandemic.
In an exciting interview, one of Loder’s questions asked: if the efficacy of monotherapies, for example, can’t be shown, then how can funding be attained? These, after all, are expensive, she said. Bingham replied that pharma, biotech, and academia all need to come up with new approaches. Then, head-to-head studies. However, she continued, pharma generally doesn’t voluntarily go down such a route. In the case of rare diseases, patients get randomised into different arms, and what is needed if every patient is going into a trial is to actually generate some data: there has to be funding for this, Bingham said.
Loder stated that well over half of investment dollars are spent on cancer. One only has to look at the statistics, she said, to see it is a relatively easy place of investment, due to the massive demand and the amount of innovation in the space.
Reimbursement and diagnostics markers
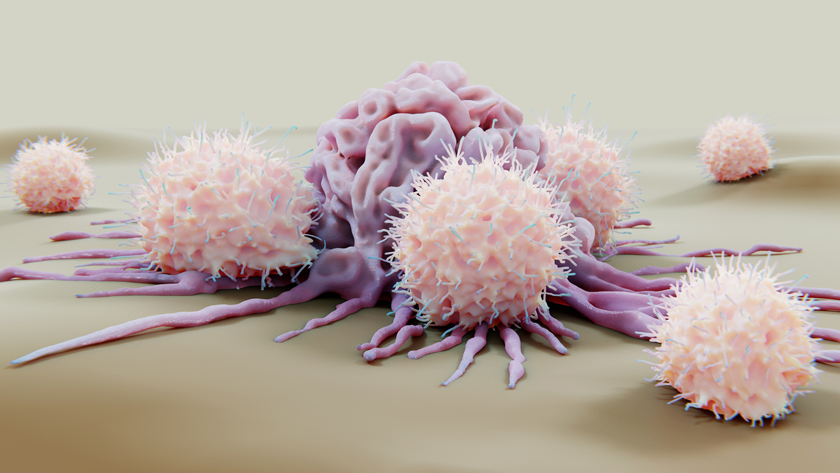
Parker Moss, chief ecosystems and partnership officer at Genomics England, spoke from the audience, mentioning how it is harder to get reimbursement for a diagnostics marker. He asked what should be done in an increasingly stratified world. Bingham replied that companion diagnostics are required. Ultimately, she said, the majority of cancer diagnoses need to be carried out much earlier on. If the clinical trial data works, she said, then early detection would be ‘a complete game changer’. She also mentioned, “vaccines before cancer even presents, before the massively hostile tumour environment”. In short, data is crucial.
Bingham continued that the Inflation Reduction Act would hit cancer patients heavily in the US as there would be a disincentive to innovate. “You’ll start your clinical trials in fifth-line, where they’ve failed all other forms of therapy,” she said. “And it takes years and years, and by that time pricing […] It’s a real concern. You can test early, but without the innovative medicines, you’re in trouble,” she warned.
Stepping up prevention – the foundation of cancer control
Following Loder’s interview with Dame Kate Bingham, the afternoon continued with another panel: ‘Stepping up prevention – the foundation of cancer control’. Moderated by Matthew Hickey, chief executive of The Health Value Alliance, panellists included: MEP Antoni Comin i Oliveres; Wendy Yared, director of the Association of European Cancer Leagues; Milka Sokolović, director-general of the European Public Health Alliance; and Marko Korenjak, president of the European Liver Patients' Association.
Hickey opened the conversation by asking what strategies are being used to reach vulnerable groups. Oliveres replied that equity must be a driving principle, particularly when it comes to cancer. So it is, he said, that public policies need to be integrated closely with the primary healthcare world and that the primary care network should be a place where prevention work is carried out. There is, he said, a paradox in the European health system, wherein budget is spent on curing illness, instead of prevention.
Summarising that it was prevention and policy – targeting the individuals at highest risk – Hickey next asked whether there was enough ambition to address inequalities. Sokolović responded that the European Cancer Plan certainly welcomes and applauds specific attention to inequalities. There are persistent discrepancies, she said, between women, elderly people, minor ethnic and racial backgrounds, and marginalised communities, all disadvantaged in different ways: more than enough reason to focus on inequalities.
From a prevention point of view, she continued, it is important to look at the variation between EU member states. For example, HPV vaccine rates in Malta are 97%; in Bulgaria, they are 2%. Furthermore, she said, for people experiencing homelessness, cancer is the second most common cause of death and there is no data for that group to help them. So, she asked in return, is the plan ambitious enough? She considered that it is, but that it depends on the extent to which member states will commit to ambitions. Only Romania and Czechia, she said, have revised their cancer policies in reaction to the plan, though.
Data is knowledge which must be shared
Hickey stated that it’s a matter of understanding the data: knowledge is power, yes, but like power, knowledge must be shared. Korenjak philosophically entered the conversation with the comparison of the water jug on the table before him: he was thirsty, but he couldn’t reach the water, and a similar experience is what is happening in Europe, he said. If you take communicable diseases and lower the cases (like hepatitis B), he said, you will directly impact the non-communicable cases (like liver cancer). A committee for health in the EU parliament would make the job easier, he noted.
Yared spoke at this point, describing how the European Cancer League is a network of cancer societies in the EU, working across the entire spectrum of cancer control. Prevention, she said, is a key area of what they do at both the umbrella and national levels. Funded by the general public, that public has to be happy. Referencing the WHO’s European Code Against Cancer, Yared highlighted the fact that 50% of cancers can be prevented by following actually very simple messages. Apart from the obvious ones like not using tobacco products, a healthy lifestyle (Mediterranean diet, exercise, and screening) – all these, she said, help. But they need translations, for example, Turkish in the Netherlands. As to whether the plan was ambitious enough, Yared reminded the panel that the EU has put cancer in a primary position before, in the 1980s. So, the important thing to focus on now is implementation.
Hickey asked what the barriers might be to implementation: Oliveres replied, the institutional merger of financial systems, and cultural barriers. Yared joined that there is a Ministry of Health, but there is also a Ministry of Finance, and cigarettes – money is derived from this. In short, Sokolović added, serious buy-in from governments is necessary; serious collaboration of commercial sectors. Also, food for prevention. Korenjak additionally thought the sharing of good practices and making systems for best practices, wherein a smarter way for distributing the budget of the EU cancer plan can be achieved.
Patient engagement and prevention on a plate
An audience member noted that money won’t work if the patient population is not engaged in stepping up for prevention. Yared agreed, stating that if populations don’t know how to reach a screening, then boots on the ground are needed to ensure awareness of screening availability. And for that, funding is required. Sokolović joined that inclusive and consistent public messaging was necessary, also.
Another audience member mentioned that Europe is very good at breakthrough, rather than follow through. There were screening recommendations back in 2003 and they have yet to be fully implemented. Yet another attendee stated that only 3% are aware of the European Code Against Cancer.
Korenjak admitted that those working in health should start with themselves, as case examples, member states offering free check-ups for different types of cancer. However, he said, lifestyle choices will always be made based on availability and access, and so education is a key first step. There need to be, he explained, financial incentives, too. Healthy food environments must be created, also.
Yared agreed: health choice must be the easy choice, she said. If people don’t have access to healthy food – “How much is lettuce compared to crisps?” she asked – then you have what is already occurring, with fast foods congregated around lower-income areas. She closed with the tale of a meeting with a supermarket chain, at which she’d wanted the European Code Against Cancer near the vegetables: they refused, stating that they had to sell everything and that they would end up having problems with certain brands.
And so, the panel came to a close, and pharmaphorum’s attendance at the event ended, prevention starting with the patients themselves a notion orbiting the minds of those within the room.













