FDA approves first cell therapy for type 1 diabetes
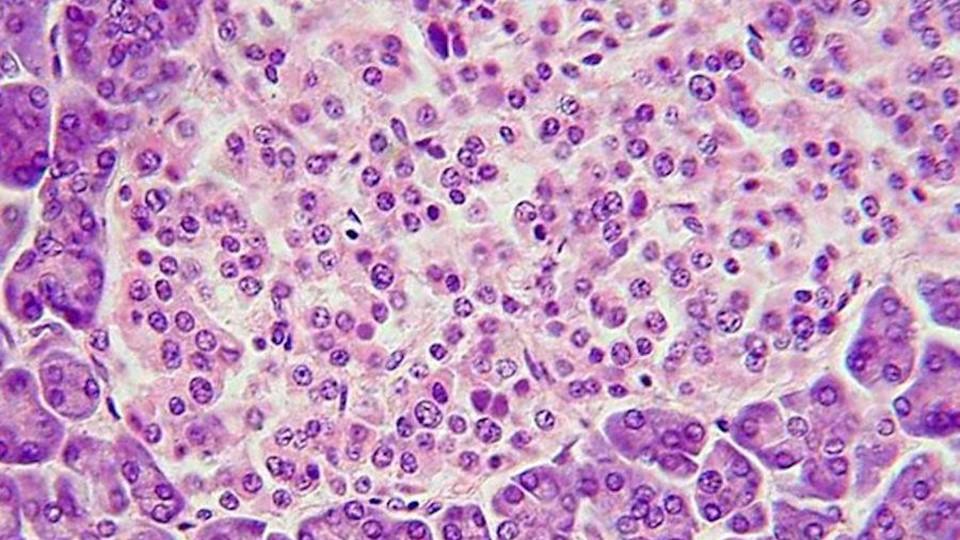
CellTrans has claimed the first FDA approval for a cell therapy used to treat type 1 diabetes, consisting of insulin-producing islet beta cells taken from deceased donors.
The Chicago-based biotech said its donislecel therapy had been approved by the FDA as Lantidra for adults with so-called ‘brittle’ type 1 diabetes, i.e. those who are unable to meet their treatment targets because they have repeated episodes of severe low blood glucose (hypoglycaemia).
The condition is very rare – affecting only around three in every 1,000 people with insulin-dependent diabetes overall – but can have a profound impact on their daily lives, contributing to anxiety and depression and raising their risk of hospitalisation and death. It is most common in women in their 20s and 30s for reasons that are not well understood.
“Severe hypoglycaemia is a dangerous condition that can lead to injuries resulting from loss of consciousness or seizures,” said Peter Marks, director of the FDA’s Centre for Biologics Evaluation and Research (CBER).
“Today’s approval, the first-ever cell therapy to treat patients with type 1 diabetes, provides individuals living with type 1 diabetes and recurrent severe hypoglycaemia an additional treatment option to help achieve target blood glucose levels.”
Lantidra aims to replace the insulin-producing beta cells in the pancreas, reducing the need for insulin injections and providing a background level of insulin secretion that can help to prevent the swings between low and high blood glucose seen in unstable type 1 diabetes.
It was tested in two open-label studies involving a total of 30 patients with type 1 diabetes who find it difficult to spot the warning signs of a hypoglycaemic episode, such as dizziness, sweating, tiredness, and a fast or pounding heartbeat.
Overall, 21 of the trial subjects did not need to take insulin injections for a year or more after infusions with the donor cells, with 11 not needing insulin for one to five years and 10 not needing insulin for more than five years. Five of the subjects were, however, unable to achieve any days of insulin independence.
While those efficacy results are impressive, there were safety issues with the procedure, which involves an infusion into the hepatic portal vein, as well as the need to take immunosuppressing medication to stop the donated cells from being rejected.
The FDA notes that “a majority” of patients treated with Lantidra experienced at least one serious adverse event and, in some cases, immunosuppressants had to be discontinued, leading to the loss of the transplanted beta cells.
The approval is, nevertheless, a regulatory landmark for cell therapy in type 1 diabetes, signalling the FDA’s willingness to approve this type of treatment at a time when other groups are working on alternatives that could sidestep the need for immunosuppressants.
Novo Nordisk recently paid $75 million upfront to partner with Aspect Biosystems’ on the development of non-donated, off-the-shelf beta cells that would be 3D printed into an encapsulated implant designed to protect them from immune surveillance, but still allow them to release insulin in response to blood glucose levels.
Also working in this area is Vertex Pharma, which has two cell therapies codenamed VX-880 and VX-264 in early-stage clinical trials. VX-880 is not encapsulated, so needs immunosuppression and could face similar issues to Lantidra, but VX-264 is an encapsulated therapy.
In new data released earlier this month, all six patients treated with VX-880 engrafted islet cells produced insulin and had improved glycaemic control, while reducing or eliminating insulin use. This week, Vertex announced a partnership with Lonza to support the manufacture of cell therapies.
The company is also working on genetically modifying beta cells to make them less likely to stimulate an immune response.
Another player, Canadian biotech Sernova, also recently reported positive results with its Cell Pouch islet cell transplant system, including insulin independence of between six and 38 months in five of the first recipients of the therapy.
Image by Polarlys via Wikimedia Commons.













