AI study will help select AFib patients for shock treatment
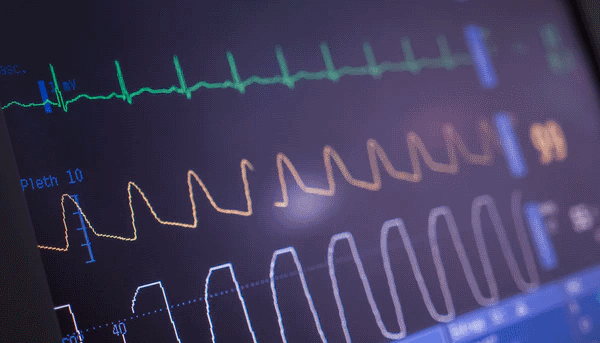
A new study is trying to find out why electrical cardioversion (ECV) or shock treatment only works in some patients with atrial fibrillation (AFib), using artificial intelligence.
The project between Cambridge based TTP plc, NHS Highland and the University of the Highlands and Islands in Scotland will apply machine learning to delve into clinical records to see if it is possible to predict whether someone with AFib should receive ECV.
AFib is a common heart condition that results in an abnormally fast and irregular heartbeat, which can put people at increased risk of complications like stroke and heart failure. It can be treated with drugs or ECV to try to restore a normal heart rhythm.
ECV has been shown to be effective in reducing complications and death from AFib, but only works in around 30% of patients at one year, according to TTP, a technology transfer firm that tries to bring scientists and engineers together on new products and technologies.
The ECV procedure also carries risk and is expensive to carry out, it says, so there is a need to predict which patients with AFib are most suitable for this type of treatment.
If effective the benefits could be considerable. AFib affects an estimated 1.5 million in the UK and 4 to 6 million in the US alone and the prevalence of AFib has been projected to increase to 15.9 million by the year 2050.
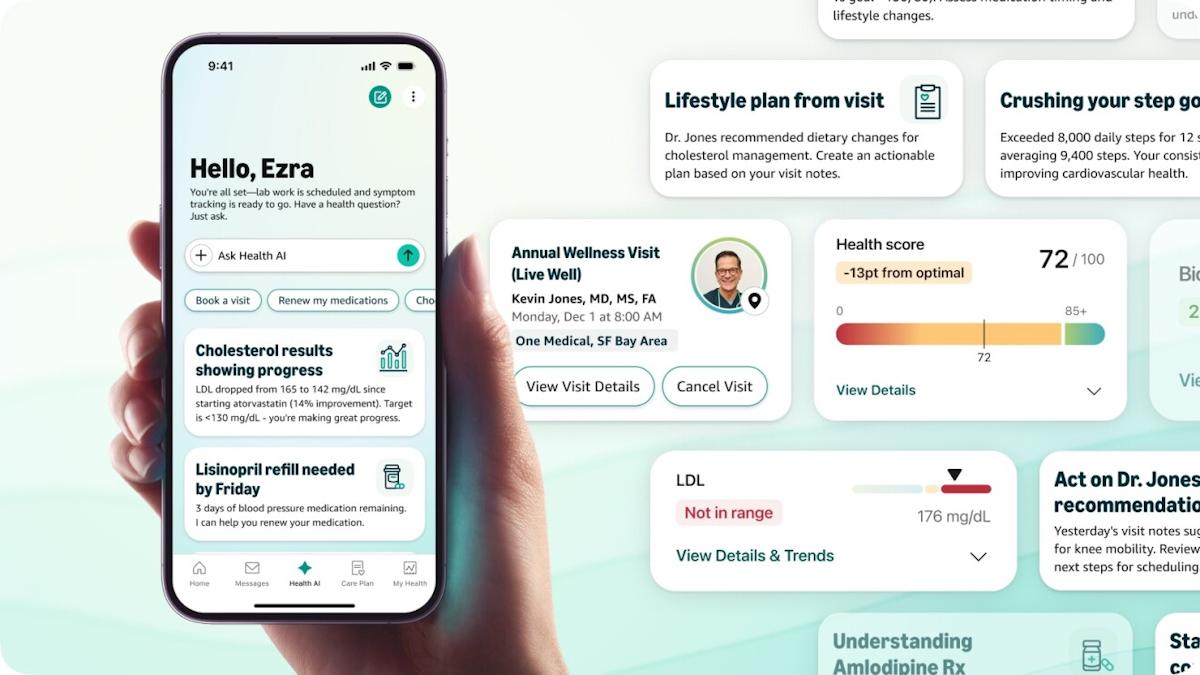
The research team will apply AI to anonymised clinical data such as electrocardiograms (ECG), patient age and gender, other illnesses, and medicine use to see if it can find patterns that influence how well patients fare after they receive ECV for AFib.
The ultimate aim is to develop algorithms that could be deployed across the NHS to try to improve clinical outcomes in AFib patients.
“Currently, decisions on whether to proceed with ECV are based on varying factors and can be fairly subjective,” said Professor Steve Leslie, a consultant cardiologist at NHS Highland.
“There is a clear need for an evidence-based test to help guide physicians when treating AFib, improve patient outcome and reduce unnecessary burden on the NHS,” he added.
2014 data from NICE suggest that AFib accounts for 0.1% of all healthcare spending in the UK, with the first healthcare cost of treating the 12,500 or so strokes caused by the condition is £148 million in the first year.
In the last few years, AFib has become a popular area of research for digital technologies and interventions.
Last year, another UK project – called STAR Mapping – was launched to apply AI to identify the causes of AFib in the hope that the insights could help patients avoid anti-arrhythmic drug treatment. Another recent AI trial based on NHS data showed that blood thinning drugs improve outcomes for all heart failure patients, regardless of whether they already have AFib.
NHS England is also putting an implantable monitor developed by medical device company Medtronic through its paces that could provide a remote early-warning system for AFib in people who have suffered a stroke of unknown cause.
Meanwhile, Johnson & Johnson and Apple have partnered on a project to investigate whether the ECG embedded in Apple Watches could be used to detect early signs of AFib, after a preliminary study reported last year backed the use of the wearable device for this application.