Hepatitis C: breaking down the stigma
David Rowlands' latest online poll examines the impact of stigma on people diagnosed with hepatitis C virus (HCV). Here he explains how breaking down perceived barriers can help reduce the spread of the virus and aid adherence to treatment.
A diagnosis of HCV has been reported to have a profound impact on social functioning. The perceived stigma associated with HCV infection leads to high levels of anxiety and exaggerated fear of transmission in patients, and can be a major cause of social isolation and reduced intimacy in relationships.
Types of infection
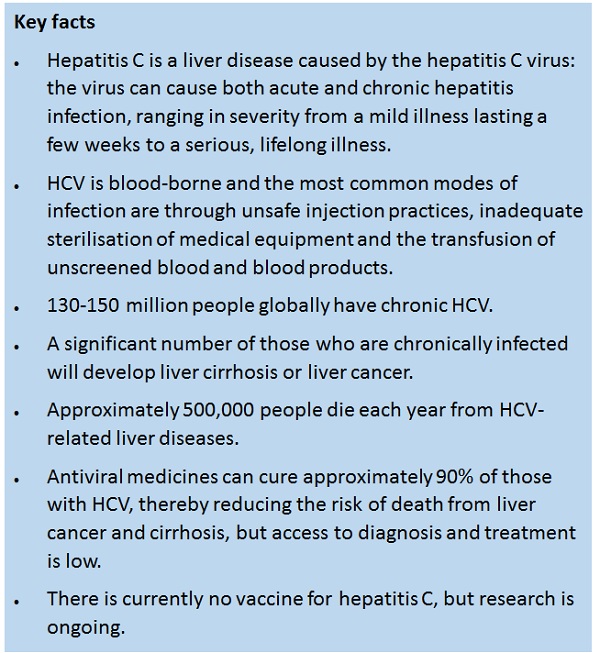
HCV causes both acute and chronic infection. Acute HCV infection is usually asymptomatic, and is only rarely associated with life-threatening disease. About 15-45% of those infected spontaneously clear the virus within six months of infection without any treatment.
The remaining 55-85% develop chronic HCV infection. Of those, the risk of cirrhosis of the liver is 15-30% within 20 years.
"Studies suggest that more than 90% of transmission in developed countries takes place through the sharing of non-sterilised needles and syringes in the intravenous drug-using populations"
Because the vast majority of people with HCV have a history of intravenous drug use, they are frequently blamed for acquiring the disease, and viewed as irresponsible, accountable and 'unworthy'. Furthermore, as a blood-borne disease, HCV is strongly associated with HIV. This association exists because intravenous drug abuse is a significant risk factor for contracting both diseases and this can be a stigmatising factor for patients.
Responding to the poll, John (57) from London, living with hepatitis C for 12 years, said, "I often attend support services and feel that there is stigma from staff and other services users about how I was infected with hepatitis C. People should take time to better understand my experiences and be non-judgmental towards me. We all have very different stories, but hepatitis C has brought us together."
Stigma can be defined as an attitude expressed by a dominant group, which views a collection of others as socially unacceptable. The notion of stigma denoting shameful relations and deviations from what is considered 'normal' has a long history within infectious disease, particularly in HIV and, more recently, in HCV.
These norms, behaviours and beliefs surrounding HCV can lead to alienation from family and friends, as well as to discrimination (perceived or real) in health services and workplaces.
"Stigma can affect self-esteem and quality of life. It can also impede the success of diagnosis and treatment, leading to continuing risk of disease transmission"
Since stigmatisation affects not only the individual but also the whole course of the disease, health care workers are not immune to stereotypes and judgements that might influence the course of the treatment of HCV patients. Changing this behaviour will help prevent patients' isolation, withdrawal of treatment and help increase the search for medical care and treatment.
Jane (36) from Manchester, living with HIV and HCV co-infection, related, "I am unable to speak with my family and friends about my health conditions. While I feel I need their support, I am unsure how I will deal with their stigma and stereotyping behaviour."
A global approach
Broad education is needed to increase understanding of this disease and should include patients and their families, health care providers and wider society. Better knowledge of Hepatitis C stigma is central to assisting patients in self-managing their illness, and it is important in reducing the disease burden.
Curing HCV chronic infection could really benefit public health by reducing the risk of complications from liver disease. Modern therapies mean the disease is curable and the efficacy of treatment markedly increases survival.
Geographical distribution
HCV is found worldwide. The regions most affected are Africa and Central and East Asia. Depending on the country, it can be concentrated in certain populations, such as among people who inject drugs, and/or in general populations. There are multiple strains (or genotypes) of the Hepatitis C virus and their distribution varies by region.
Treatment
HCV does not always require treatment as the immune response in some people will clear the infection, and some people with chronic infection do not develop liver damage. When treatment is necessary, the goal of treatment is cure. The cure rate depends on several factors, including the strain of the virus and the type of treatment given.
The standard of care is changing rapidly. Until recently, it was based on therapy with interferon and ribavirin, which required weekly injections for 48 weeks, cured approximately half of treated patients, but caused frequent and sometimes life-threatening adverse reactions.
"Much needs to be done to ensure that medical advances lead to greater access to treatment globally"
Recently, new antiviral drugs have been developed. These direct antiviral agents (DAA) are much more effective, safer and better-tolerated than the older therapies.
Therapy with DAAs can cure most people with Hepatitis C infection and treatment is shorter (usually 12 weeks) and safer. Although the production cost of DAAs is low, the initial prices are very high and likely to make access to these drugs difficult even in high-income countries.
Poll data
Members of the community were asked their views on the stigma of living with hepatitis C. There were 57 respondents between 1 December and 14 December 2015, with views collected via online hosting at www.Design-Redefined.co.uk and social networking sites. Thanks to all those who shared their views.
Click here to take part in the next poll.
About the author:
David Rowlands is the director of Design-Redefined.co.uk, delivering effective healthcare communications to enable people with HIV and/or hepatitis C (HCV) to become better engaged with their treatment and care.
Drawing on his established networks and collaboration with partners, David is able to bring healthcare together, by engaging patients and organisations, healthcare providers, physicians, stakeholders and policy makers.
Contact David via Email: david@design-redefined.co.uk Website: http://www.design-redefined.co.uk Twitter: @DR_tweetUK
Read more from David Rowlands:
Examining the WHO guidelines on HIV testing services
Copyright statement:
This article is for use online at www.pharmaphorum.com only. Articles may be redistributed in other media and non-commercial publications with the consent of the author. Any republication must acknowledge the author with a link back to www.design-redefined.co.uk. The author may request compensation for republication of any unauthorised content.










