Expanding research capacity into neglected tropical diseases
Professor Paul Kaye from the University of York, whose research team was recently granted €8 million to help reduce the burden of leishmaniasis in African countries, takes us through the long but rewarding process of developing a vaccine for a neglected tropical disease.
Neglected tropical diseases (NTDs), of which there are 19 according to the World Health Organization (WHO)1, together affect more than one billion people across 149 countries worldwide. Developing effective therapies has achieved some success (six of the 19 are considered treatable), but there are still volumes more work to be done, all across the globe.
My own research has focused on the leishmaniases, a family of devastating vector-borne diseases, affecting people across East Africa, Asia, the Middle East, and Central and South America2.
As with most NTDs, the leishmaniases affect the poorest, most malnourished individuals, and contribute to a vicious cycle of poverty and disease. They present significant risks to public health, both physical and mental, and to socioeconomic development.
The leishmaniases broadly fall into two categories: tegumentary leishmaniases (TL), affecting the skin and mucosa, and visceral leishmaniasis (VL), targeting the internal organs.3,4 Within TL, there are three subtypes: self-healing lesions at the bite location (cutaneous leishmaniasis; CL), lesions that spread from the original lesion to the mucosae (mucosal leishmaniasis; ML), and those that spread across the body (disseminated or diffuse cutaneous leishmaniasis; DCL).
Visceral leishmaniasis, also known as kala-azar, involves the major internal organs; patients recovering after drug treatment often develop post kala-azar dermal leishmaniasis (PKDL), a chronic skin condition in which nodular or macular lesions begin on the face and spread across the trunk and arms. Since PKDL may develop in up to half of patients treated and apparently cured from VL, it is thought to play a central role in community transmission.5
There are over one million new cases of TL and half a million new cases of VL each year, which together translate into some 2.4 million disability-adjusted life years.4 True prevalence may be even higher, as the diseases often affect dispersed or nomadic populations. The significant physical marks that are often the aftermath of the diseases may have a long-lasting impact on mental health and perpetuate social stigma associated with the disease.6
The past challenges of treatment — and new promise
The leishmaniases have historically been difficult to treat, due both to the limited access to healthcare faced by at-risk populations and the fact that the small battery of existing drugs has increasingly succumbed to resistance.
Additionally, because the cells in question are eukaryotic, they are similar to human cells — so toxins capable of killing them can be harmful, or fatal, to pathogen and host alike.
Although the burden of VL in South Asia has been curtailed somewhat by single-dose liposomal amphotericin B, the drug is less effective in other geographic locations, namely East Africa. Various drug combinations have been tested, unsuccessfully, while new therapies and immune modulators in early stage development are as yet untested in the field. Sadly, not much has changed in the treatment for CL over the past fifty years.3 The only approved vaccine to date is for canine visceral leishmaniasis.
Thirty years of discovery science has led to the development of a candidate for a therapeutic vaccine for PKDL, the mysterious sequela to VL.7 My team, including colleagues from Sudan, have been intimately involved in this work and are in the midst of a phase IIb clinical trial funded by the Wellcome Trust, evaluating the efficacy of this therapeutic vaccine in Sudanese patients with persistent PKDL.8,9
But the research has a long journey behind it, and at least as far to go. To expand the research, we developed a research consortium with colleagues in Ethiopia, Kenya and Uganda and at the European Vaccine Initiative (EVI) in Germany, to evaluate the immune status of people suffering from leishmaniasis.
We’ve also received a grant from the European & Developing Countries Clinical Trials Partnership (EDCTP) that will allow us to not only extend our vaccine programme in Sudan,10 but also to address other important research challenges faced by the medical community in remote locations. Our larger aim has been to develop a “blueprint” laying out the basic strategy and research tools needed in our project, in the hopes that our work will extend far beyond leishmaniasis to help researchers address other NTDs around the world.
Developing the tools to find a vaccine
To design new treatments, researchers first need tools capable of taking “before and after” snapshots of immune system changes - in other words, a comparison between the state of the immune system when a patient is first admitted to hospital and when the patient is cured with treatment. By understanding these often tiny alterations in immune cells, we can design ways to improve how treatments work in concert with the cells, and even understand why some patients may relapse from their disease or develop PKDL.
Flow cytometry has been a critical tool to uncover mechanisms of immunity, assessing how well vaccines work as well as the biomarkers of drug response. It uses antibodies that recognise specific markers on the surface or inside immune cells, which help us predict their function. These antibodies are fluorescently labelled, and by exposing each cell individually to laser light as they pass through a small aperture, the fluorescent signal can be detected.
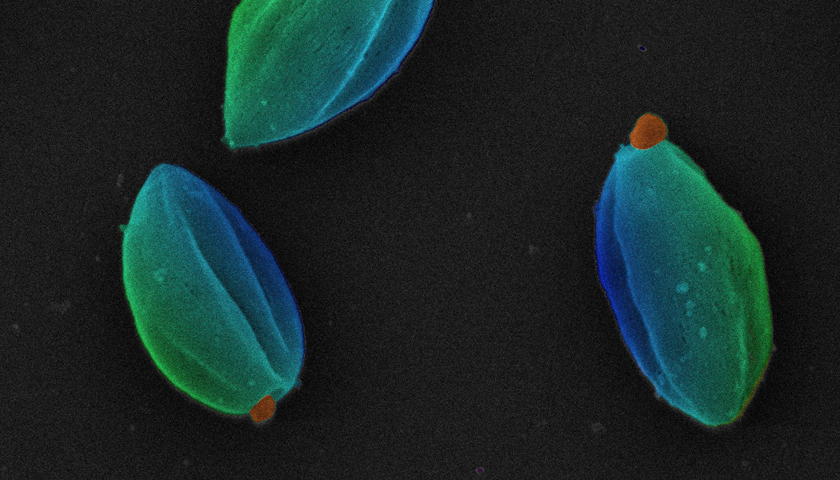
[caption id="attachment_69719" align="aligncenter" width="619"] Initial training course with recently appointed flow managers (Credit: Dr Karen Hogg, University of York). Image at top of page: Leishmania mexicana parasites in the amastigote stage, SEM. Credit: University of Oxford, Richard Wheeler. Attribution 4.0 International (CC BY 4.0)[/caption]
Initial training course with recently appointed flow managers (Credit: Dr Karen Hogg, University of York). Image at top of page: Leishmania mexicana parasites in the amastigote stage, SEM. Credit: University of Oxford, Richard Wheeler. Attribution 4.0 International (CC BY 4.0)[/caption]
For our project, we needed several attributes in a flow cytometry instrument: it had to be sufficiently sensitive to identify rare cell populations, often with low levels of biomarker; it had to provide extreme reproducibility between sites (i.e. inter-machine reliability); and it needed to be manufactured by a company offering service support across a large geographic region. We settled on CytoFLEX, a research flow cytometer that uses avalanche photodiode detection to arrive at the required level of sensitivity.
With assistance from CytoFLEX’s developer, Beckman Coulter Life Sciences, we’ve devised and run initial training courses with a group of newly designated flow managers from each partner country, to share standard operating procedures, develop high-level data analysis strategies, and offer instruction in routine maintenance.
Beckman Coulter Life Sciences also provided freeze-dried antibody cocktails (DURAClone panels). For investigators in remote locations, the use of dry, pre-formulated reagents, rather than “wet” antibodies, solves some logistic problems. Additionally, the use of DURAClone panels removes a number of sources of variability and increases sample throughput12.
Through these avenues and innovations, we’ve established a new network for flow cytometry in East Africa that will allow us to identify and characterise the immune cells present in the blood during these devastating diseases. We will match our current data with similar techniques in pathology, to compare blood immune cell profiles with those of cells found in the skin, and give a more complete picture of the host response to infection before and after treatment or vaccination.
The efficacy trial of our therapeutic vaccine, ChAd63-KH, is well underway (therapeutic vaccines are given after an individual is infected with a pathogen and designed to bolster the immune system and eliminate the infection). The technology, similar to the University of Oxford’s promising COVID-19 vaccine candidate, introduces two genes from Leishmania parasites (KMP-11 and HASPB1) into a well-studied chimpanzee adenovirus (ChAd63 viral vector). After vaccination, host cells become infected with the virus and express the Leishmania proteins in a way that can be recognised by the immune system. We are especially interested in how well this vaccine can generate T cells to fight the infection.
The next immediate goal, funded by EDCTP, is to commence a clinical trial to determine whether the vaccine can prevent progression from VL to PKDL. Finally, we hope to develop a human challenge model of leishmaniasis to test the vaccine’s ability to protect against infection by different forms of parasite. This would pave the way for the development of a cost-effective prophylactic vaccine, which is the real goal in order to prevent these diseases occurring in vulnerable populations in the first place.
Future directions
As mentioned, our research also has larger ambitions for global public health over the long term. Our East African partners are linked together through their work as members of the Leishmaniasis East Africa Platform group, established to help coordinate drug development activities in the region by the Drugs for Neglected Diseases initiative (DNDi). Central questions about why the disease varies between countries are being studied, and the increased capacity for flow cytometry will additionally support patient monitoring in drug trials conducted by DNDi and other research groups.
And through the capacity-building this project provides, we hope its reach will extend far beyond leishmaniasis, to provide support for research into other NTDs, including bacterial, fungal, and other parasitic and viral diseases.
We are also conducting supporting work, which will make a case for the future financial investment necessary to make these vaccines available to those who need them, in part by modelling the impact vaccines might have on health outcomes.11 By continuing to demonstrate the analytical power of methods like flow cytometry and their roles in helping design much-needed therapies for the NTDs, we hope to open additional discovery research possibilities for colleagues in many parts of the world.
The research described in this article is part of the EDCTP2 programme supported by the European Union (grant number RIA2016V-1640; PREV_PKDL; https://www.prevpkdl.eu).
About the author
Paul Kaye is professor of immunology at the University of York
References:
- World Health Organization: https://www.cdc.gov/globalhealth/ntd/diseases/index.html. Accessed 8 June 2020.
- World Health Organization: https://www.who.int/en/news-room/fact-sheets/detail/leishmaniasis. Accessed 8 June 2020.
- Kaye PM, Cruz I, Picado A, Van Bocxlaer K, Croft SL. Leishmaniasis immunopathology-impact on design and use of vaccines, diagnostics and drugs. Seminars in immunopathology. 2020;1-18
- Drugs for Neglected Diseases initiative: https://www.dndi.org/diseases-projects/leishmaniasis/. Accessed 8 June 2020.
- World Health Organization: https://www.who.int/leishmaniasis/en/. Accessed 8 June 2020.
- Pires M, Wright B, Kaye PM, da Conceição V, Churchill RC. The impact of leishmaniasis on mental health and psychosocial well-being: A systematic review. PLoS One. 2019;14(10):e0223313.
- Mukhopadhyay D, Dalton JE, Kaye PM, Chatterjee M. Post kala-azar dermal leishmaniasis: an unresolved mystery. Trends Parasitol. 2014;30(2):65‐74.
- ClinicalTrials.gov: https://clinicaltrials.gov/ct2/show/NCT03969134. Accessed 8 June 2020.
- Wellcome: https://wellcome.ac.uk/what-we-do/directories/translation-fund-projects-funded. Accessed 8 June 2020.
- ClinicalTrials.gov: https://clinicaltrials.gov/ct2/show/NCT04107961. Accessed 8 June 2020.
- Le Rutte E, Coffeng L, Malvolti S and Kaye PM, de Vlas, S. The potential impact of human visceral leishmaniasis vaccines on population incidence. Preprint published online. https://doi.org/10.1101/2020.05.05.20090480. Accessed 12 June 2020.
- Rajab, A, Axler, O, Leung, J, Wozniak, M, Porwit, A. Ten‐color 15 antibody flow cytometry panel for immunophenotyping of lymphocyte population. Int J Lab Hem. 2017; 39(Suppl. 1): 76– 85.












