Is a lack of real-time data holding trials back?

It’s 2020 and the digital revolution is well on its way. Yet, for clinical trials worldwide, real-time access to data is not the norm – and that lack can create a cascading set of issues affecting every aspect of a study.
Critical decisions are too often being made in a digital data vacuum. At best, processes are not as efficient as they could be; at worst, serious problems may go undetected for weeks or even months.
As the amount and types of data expand exponentially, this problem only intensifies. Yet, ironically, that very growth in data sources may be one reason solutions have been slow to take hold.
In a recent analysis, the Tufts Center for the Study for Drug Development reported that more than two-thirds of all sponsors are using at least four different data sources. They find the tasks related to rendering that data usable – importing and ingesting data, transforming and mapping data, cleaning, and reviewing data – to be extremely time-consuming. That slows use. Worse, they also find initiating relationships with data vendors to be extremely time-consuming, so iterating to new technological solutions can feel daunting.
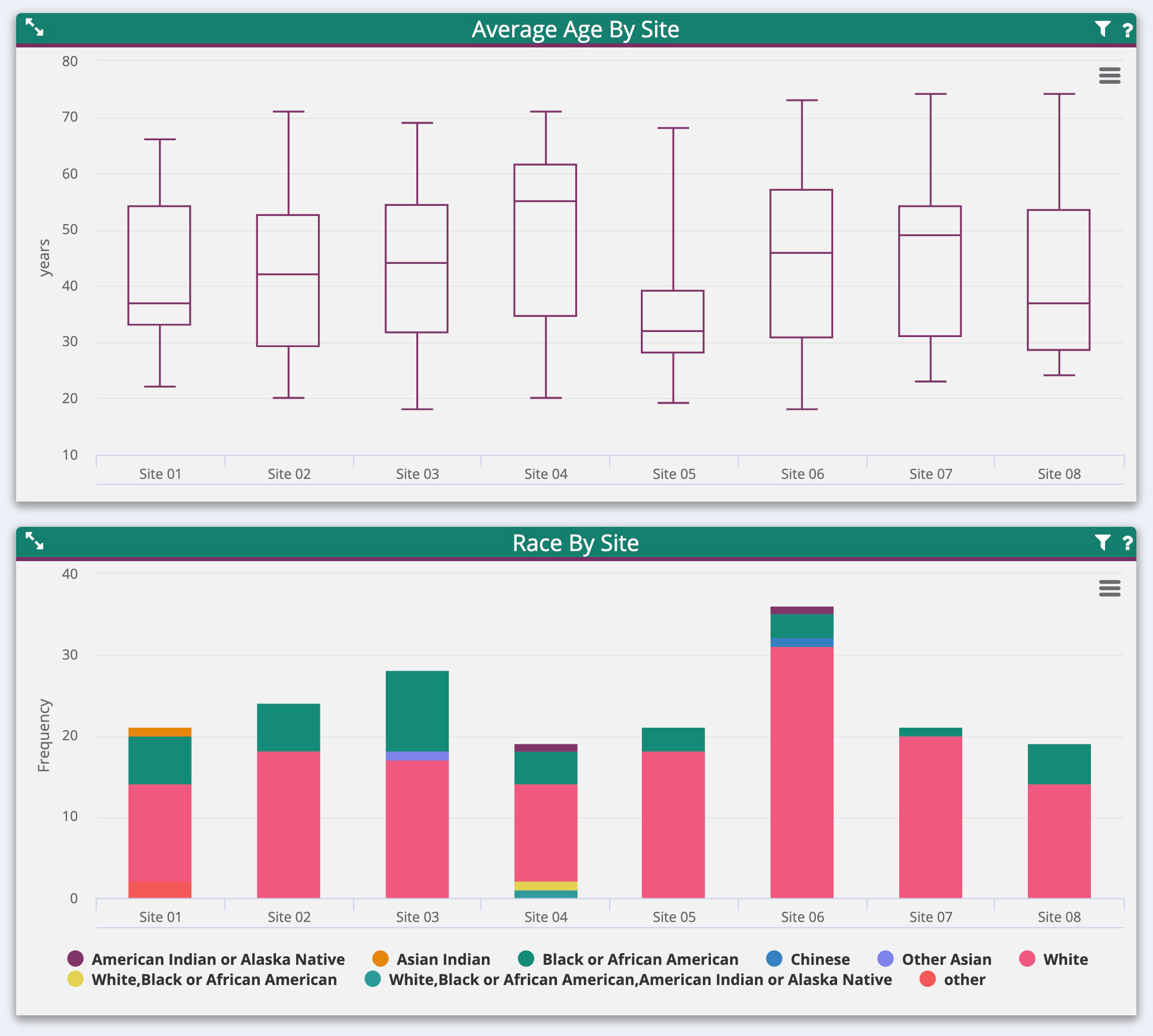
What does this mean for clinical trials? Analysts at Pharma Intelligence decided to find out, surveying professionals involved in clinical data management. Their pool of 155 respondents comes from large pharma companies, biotech companies, device developers, and contract research organisations worldwide. Their findings, published in the September 2018 research report Challenges and Opportunities in Clinical Data Management, underscore the severity of the problem.
Delayed data delivery
Study data is typically collected by internal and external partners. Researchers rely on these partners to distribute their findings in a useable format, which often only occurs once the data has been specifically requested. Frequently, this distribution can take up to 10 weeks – and sometimes it does not happen until after a trial is complete.
The Pharma Intelligence survey showed that 62% of respondents do not get their data in real-time.
As much as 13% of biomarker data may not be available until post-trial, eliminating its value in developing and delivering personalised precision medicine. While electronic data capture (EDC) produces the swiftest overall data distribution, 6% of the time even EDC data is still not delivered until after trial completion¹.
Yet mHealth and the Internet-of-Things cause the greatest trepidation among researchers. Today, only 7% of those results are reported the same day and over half of the reportable data takes between two and ten weeks to reach researchers. This in itself is troublesome – but as trials become increasingly decentralised and researchers rely more and more on digital health tools and patient-generated data, the problem will only be exacerbated. Indeed, handling such data and finding resources to clean and manage it was overwhelmingly cited by Pharma Intelligence respondents as the most urgent challenge facing researchers over the next five years.
Potentially catastrophic setbacks
When data delivery lags behind the pace of the trial, data entry is delayed – especially when data arrives in multiple formats and from different sources that need to be reconciled. Clearing redundant data then becomes difficult, and programming complex edit checks becomes impossible.
The lack of timely data wastes time and may require costly Corrective Action/Preventive Action (CAPA) programmes, causing even more expensive delays in trials. An even worse outcome is that data verification is hindered. Researchers are unable to ferret out missing and inconsistent data, sometimes with serious consequences. External and internal audits, when performed, typically reveal source document discrepancies, informed consent issues and lack of drug accountability.
Such information is used to reveal protocol or enrolment issues; indeed, 25% of survey respondents said they have paid for patients who should not have been in their trials because they received the data too late¹. If some results are severely skewed, and only uncovered when data is delivered post-trial, the entire clinical trial may have to be rerun, at a colossal cost of time and money.
New technology insights
Ironically, the need for greater data insight coincides with the rise of digital technologies that can track results in real-time. The hurdle lies in transferring those results to the sponsor swiftly and in a useable format. Fortunately, there are technological solutions for that, too, and such real-time data synthesis and analytics will transform clinical trials.
Researchers need to be able to act quickly and decisively to protect patient safety when exploring next-generation therapies — biologics, cellular, and genetic modification treatments. Furthermore, companies want to eliminate both hard costs and errors, and technology can enable sponsors to dramatically reduce trial expenses several ways, namely through the use of:
- Richer, more frequent data sets could support smaller patient sample sizes
- Workflow management tools to increase process efficiency and reduce waste
- Early, educated decision-making to inform mid-trial redesigns or termination.
So why have such systems not been universally adopted? Previous solutions have involved a host of barriers, from high up-front costs and complex technology integrations to a simple fear of change on the part of sponsors and CROs. That’s all changing and modern systems should eliminate those concerns by easily adapting to the current IT environment and minimising the need for costly change management.
A real-time revolution for clinical trials
Delays in data transfer from external and internal partners have long been an expected inconvenience in the course of a clinical trial – one that is becoming untenable as the amount and variety of trial-related data multiplies. Unable to view or verify data, researchers face errors, delays, inefficiencies and costs that should be entirely avoidable.
By adopting new technology solutions, sponsors, and CROs can change this scenario. They can glean real-time insights – and revolutionise their clinical trials. Data quality will improve, decision-making will be more informed, trial timelines and costs will shrink, and patient safety will be more secure.
This is all good news for pharma companies and could shift the productivity and economics of their business. Most importantly, however, these advances could mean that life-changing new therapies reach patients years earlier. That’s transformative.
References
1. Challenges And Opportunities In Clinical Data Management RESEARCH REPORT 2018 by: Pharma Intelligence
About the author
 Michael Arlotto is president and co-founder of Remarque Systems. Michael is an industry leader who understands the key business drivers to generate value, with more than 25 years of scientific, investment and operational experience in pharmaceutical, biotechnology, pharmaceutical service, and healthcare IT industry.
Michael Arlotto is president and co-founder of Remarque Systems. Michael is an industry leader who understands the key business drivers to generate value, with more than 25 years of scientific, investment and operational experience in pharmaceutical, biotechnology, pharmaceutical service, and healthcare IT industry.