Why the ‘80/20 Rule’ does NOT rule the specialty pharmaceutical industry
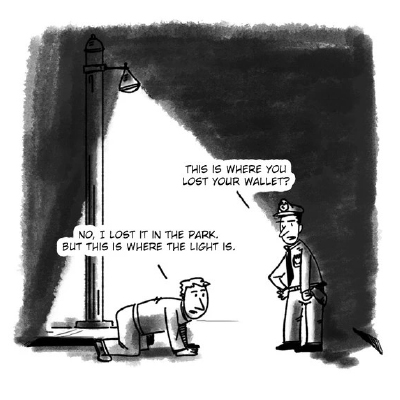 A joke is told about a drunk man who loses his wallet in the park, but for some reason is searching for it under a streetlight. When asked why he is searching there, the drunk replies, "This is where the light is." The so-called “streetlight effect” and its associated biases are well-documented, even in scientific fields.
A joke is told about a drunk man who loses his wallet in the park, but for some reason is searching for it under a streetlight. When asked why he is searching there, the drunk replies, "This is where the light is." The so-called “streetlight effect” and its associated biases are well-documented, even in scientific fields.
When working with drug manufacturers to optimise therapy onboarding, we can observe a similar pattern: 80% of patient services budgets are spent on only 20% of patients. Which patients are those? Those “under the streetlight,” who were motivated and proactive enough to enrol in the Hub.
Building a robust Hub model
For specialty drug manufacturers, the gold standard for patient support services has revolved for many years around the Hub. One industry insider estimated manufacturers will spend a combined $25 billion on Hub services this year. We accept this as the cost of doing business in 2023 as a best practice for solving the most pressing obstacles for patients looking to obtain therapies: access and affordability.
Building a robust Hub model is one of the most basic parts of the industry-standard playbook for launching a new specialty drug. However, that playbook fails to account for a critical question: How can manufacturers optimise their therapies when the majority of those who receive a new prescription never enrol in Hub services? For all the time and money manufacturers spend to support patients, anecdotally speaking, about 20% of those who receive new prescriptions actually enrol in Hub services. But what about the other 80%?
With all the focus and attention on the Hub, there are many reasons why it is so underutilised. First, according to Accenture, 87% of patients are unaware that patient support services exist for their therapy. Second, the proliferation of services has created more complexity for physicians to navigate, so many prescribers offer little assistance to patients after writing the prescription. Third, Hub enrolments require prescribers to collect legal consents from the patient right after the prescription is written.
Efficiency, efficacy, and timely communication
Beyond that, information is often lost in translation between patients, physicians, clinics, and the Hubs - leading to further delays. The cost of this lost time is clear: the longer the period between prescription and enrolment, the higher degree of abandonment can be expected. Getting through these critical first steps is easier when providers are able to interact with a patient face-to-face. However, face-to-face interactions are fewer and fewer as appointments go virtual and providers struggle to keep up with patient demand. To enrol a patient in hub services today requires efficient, effective, and timely communication.
Therein lies another challenge: the doors are quickly closing on our attention. People are highly sensitive to the friction points along the journey to the Hub, whether that means answering a phone call from an unknown number (94% are not picked up), opening an email (79% are never opened), or installing an app (which 78% abandon). Smartphones offer the convenience of on-the-go communication, but those who rely on a patient’s mobile number or email address must compete with every other digital marketer vying for a patient’s attention. Ineffective digital communication is a problem, rather than a solution, for manufacturers who try to enrol new patients in their Hub. It doesn’t matter how much your drug helps them avoid the next seizure, the next flare-up ― if you can’t reach patients at the right moment, they will be lost.
The upshot is this: patient support services spend all their time focused on the 20% of patients who have made it to the hub ― those who have effectively raised their hand and asked for help. The other 80% are left to fend for themselves. Understanding why these patients get lost along the way is critical to getting them the help they need. Unfortunately, many manufacturers struggle with how to improve the therapy enrolment process that allowed these patients to get lost in the first place.
Searching the dark part of the pavement
Looking to your Hub for solutions is no different than losing your keys whilst walking on a dark pavement, and looking only under the streetlight to find them. Even though your keys are more likely in the dark (the part of the journey before the Hub), this is the hardest area to search and thus is often ignored.
Everyone should reap the benefits of the industry’s $25 billion investment in patient support services. Right now, it only goes to the 20% who enrol, while the other 80% are left in the dark ― what I call the 80/20 fallacy. The pharmaceutical industry is, in effect, operating under the opposite of the Pareto Principle, a concept from economics that states that by investing just 20% of our effort, we can achieve 80% of the overall result. For the remaining 20% of the result, 80% input is needed. This is why this principle is often referred to as the 80/20 rule.
Following the opposite rule is not a recipe for long-term success. Specialty drug manufacturers cannot continue to squander their patient services money on a minority of their patients. The industry faces an inflection point around one of two paths: finding a better way to enrol more patients in the Hub, or to continue under-investing in the majority of its customers.












