As WHO calls mpox emergency, NIH says only drug ineffective
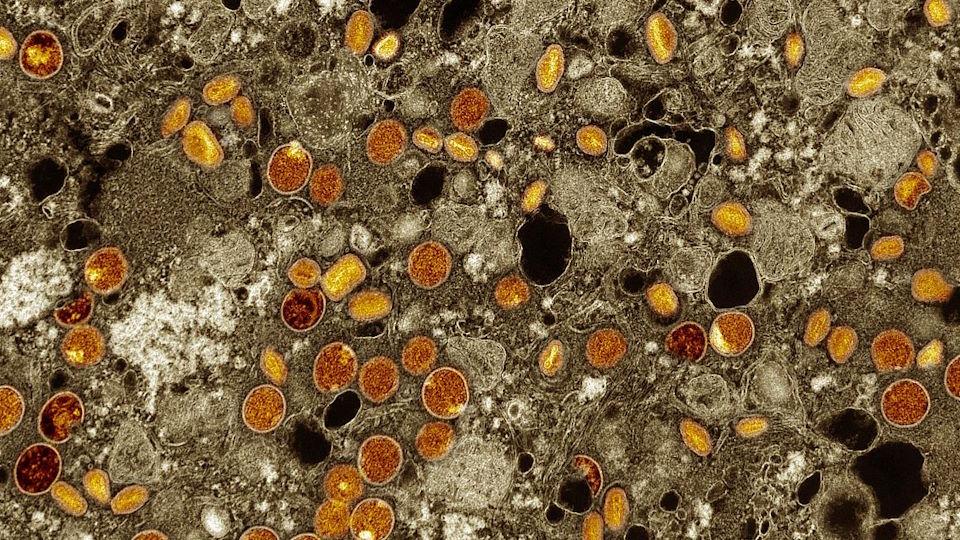
Colourised transmission electron micrograph of mpox virus particles (red/yellow) found within infected VERO E6 cells (brown).
The only antiviral recognised as an mpox treatment was unable to shorten the time to resolution of lesions in a trial in the Democratic Republic of the Congo (DRC), the epicentre of an outbreak deemed a public health emergency by the WHO yesterday.
An initial analysis from the PALM 007 study carried out by researchers from the US National Institutes of Health and DRC's Institut National de Recherche Biomédicale (INRB) concluded that tecovirimat – sold as TPOXX by US drugmaker SIGA – was no better than placebo at mitigating mpox symptoms and preventing serious outcomes, including death.
TPOXX is approved for smallpox, but has been used off-label to treat mpox (formerly known as monkeypox), which is in the same virus family, in many countries.
The antiviral was also cleared in the EU in 2022 for the treatment of mpox under exceptional circumstances, during the outbreak of less virulent Clade II infections that followed the COVID-19 pandemic. The NIH/INRB trial, however, is focusing on the Clade I strain of mpox that is endemic in Central Africa.
A variant of that strain – known as Clade Ib – is responsible for a surge in cases in DRC, as well as countries where it is not normally endemic, including Burundi, Central Africa Republic (CAR), Kenya, Rwanda, and Uganda. The Africa Centers for Disease Control and Prevention (Africa CDC) declared a public health emergency earlier this week, and the WHO followed suit shortly afterwards.
"The emergence of a new clade of mpox, its rapid spread in eastern DRC, and the reporting of cases in several neighbouring countries are very worrying," according to WHO Director-General Dr Tedros Adhanom Ghebreyesus.
"On top of outbreaks of other mpox clades in DRC and other countries in Africa, it's clear that a coordinated international response is needed to stop these outbreaks and save lives."
One promising finding from the trial was, however, that the mortality rate for enrolled subjects was 1.7% – less than half the 3.6% rate reported among DRC cases overall – which the researchers said shows that better outcomes among people with mpox can be achieved when they are hospitalised and provided high-quality supportive care.
Overall, mortality was lower, and lesions resolved faster than anticipated – regardless of whether participants received tecovirimat or placebo, according to the NIH.
Tecovirimat was found to be safe, but the efficacy result is disappointing, said Jeanne Marrazzo, director of the NIH's National Institute of Allergy and Infectious Diseases (NIAID).
She added, however, that the findings "give us essential information and reinforce the need to identify other therapeutic candidates for mpox while we continue research on tecovirimat use in other populations with mpox."
The NIH is running another trial called STOMP in the US in people with lab-confirmed or suspected mpox infections, also focusing on time to clinical resolution of skin lesions. Meanwhile, a similar study called UNITY is running in Argentina, Brazil, and Switzerland.
While the new study is a blow – given that tecovirimat remains the only recognised drug treatment for mpox – there are three vaccines available to help fight the outbreak, which has resulted in 17,000 reported cases and 500 deaths across Africa.
Bavarian Nordic's Jynneos/Imvanex/Imvamune is approved in the US, Europe, and Canada, while KM Biologics' LC16 vaccine is available in Japan and Emergent BioSolutions' ACAM2000 is under regulatory review for mpox in the US, according to GlobalData.
"Procurement of vaccines to distribute to populations most at risk should now be a key priority in order to contain the outbreak and save lives," said GlobalData's associate director of infectious diseases, Fiona Chisholm.
"Mpox vaccines played an important role in containing the 2022 mpox outbreak in high-income nations, but none are currently widely available in Africa."
The European Commission has already said that it will donate 175,420 doses of the Bavarian Nordic shot to the Africa CDC.
The company has pledged to donate 40,000 doses and has confirmed it can produce the 10 million doses sought by Africa CDC by the end of 2025, and is waiting to receive orders, but those numbers suggest vaccine supplies will be in "extremely short supply […] at least in the near term," said Chisholm.











