NHS reimburses Roche's Hemlibra in new group of haemophilia patients
NHS England has agreed to reimburse Roche’s Hemlibra (emicizumab) in a new group of patients with haemophilia A, widening access to the potentially life-saving drug.
Following the commissioning decision by NHS England, around 2,000 people with severe congenital haemophilia A without factor VIII inhibitors will be eligible to receive the drug.
This includes many young children whose parents sometimes struggle to administer the current infusion several times a month.
NHS England already funds Hemlibra for patients with inhibitors, okaying reimbursement in July last year.
Hemlibra received a marketing authorisation from the European Medicines Agency for prevention of bleeding episodes in people with severe congenital haemophilia A without factor VIII inhibitors in March 2019.
The drug was commissioned directly through NHS England Specialised Services, which focuses on funding decisions for very rare diseases.
NHS England said the treatment is part of a package of measures outlined in the NHS Long Term Plan, focusing on providing access to advanced medical interventions that can save lives.
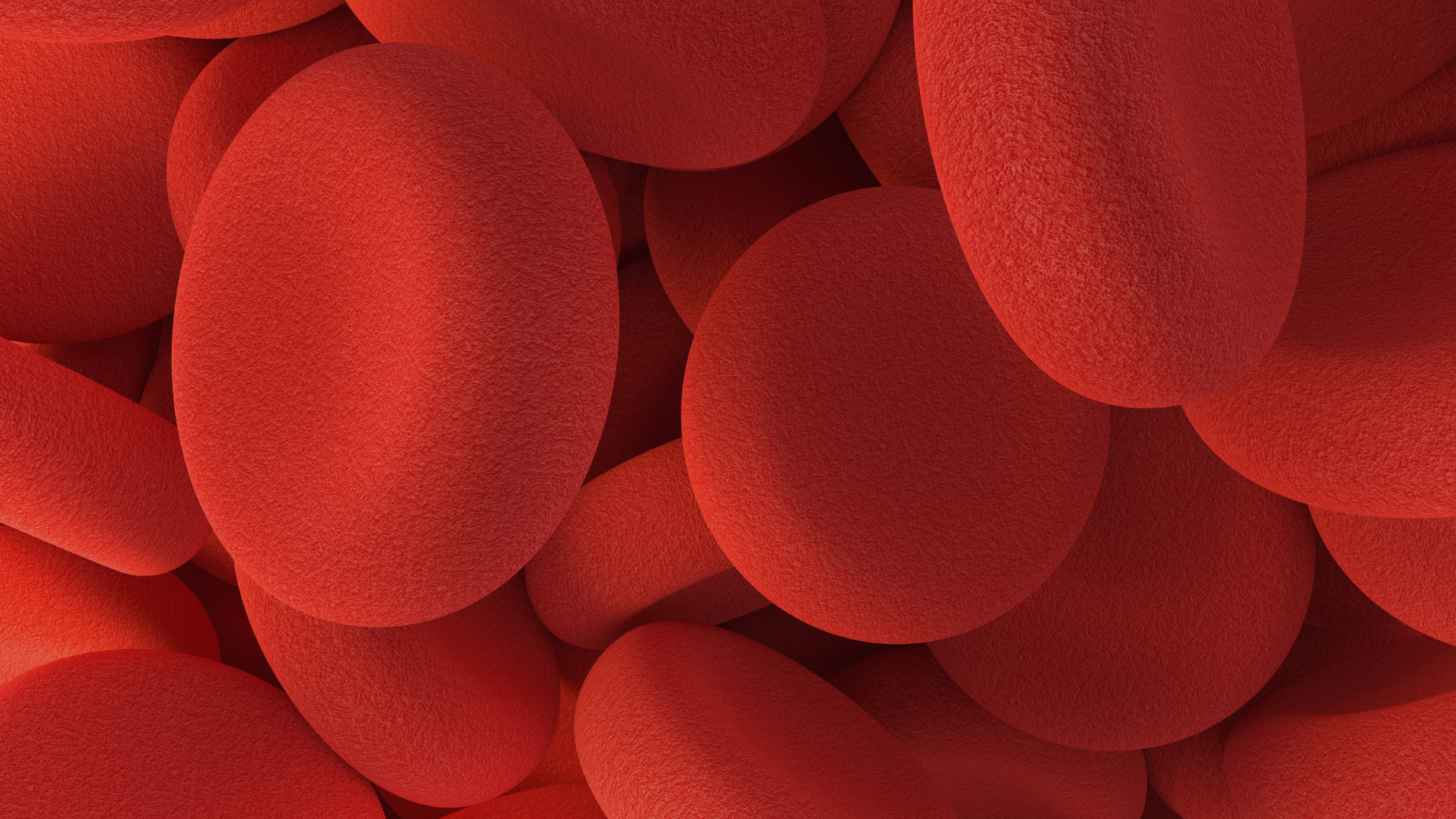
The condition means that even a cut or graze could lead to uncontrolled bleeding that can cause serious harm and even death.
Hemlibra works by mimicking the action of the blood protein factor VIII, and as a fortnightly injection it negates the need for multiple time-consuming infusions every week.
NHS chief executive Simon Stevens said: “Giving patients access to world class, trailblazing drugs and therapies is a key part of the NHS Long Term Plan which aims to save thousands more lives.
“This treatment has the potential to significantly improve the lives of people with haemophilia, especially children – reducing treatment time and even ending the dangerous bleeds which can lead to life-threatening cuts and life-changing damage.”
Liz Carroll, chief executive of The Haemophilia Society, said: Current treatments can require intravenous infusions multiple times a week which can place a significant burden on people with haemophilia and their carers. This decision will mean that people will have the opportunity to have treatment less frequently without intravenous access which will enable many to live their lives more freely.’’












