Robots don't improve prostate surgery outcomes, says study
The advantages of using robotic surgery to treat prostate cancer have been called into question after a study examined its long-term benefits compared to traditional surgery.
Experts aren't writing off the technology yet, as the study found signs it is better for patients in the short term - however its high cost is a concern.
The study is the first ever to directly compare the surgical methods. Robotic surgery for prostate cancer has been rapidly adopted in the US where around 80-85% of prostatectomies are performed using robotic assistance, though uptake in the UK and Europe has been much slower.
The randomised, controlled study, published in The Lancet, investigated the impact of both robotic and non-robotic approaches on quality of life outcomes in men with the disease who have their prostate surgically removed.
The results come from the first stage of a two year trial and include outcomes such as urinary and sexual function.
A total of 308 participants were included in the study and were randomly assigned either robotic surgery (157) or open surgery (151).
No differences in urinary or sexual function, post-operative complications and number of days away from work were reported after the 12 week follow-up period.
There were differences in the length of hospital stay after surgery (longer after open surgery), blood loss during surgery (more with open surgery), pain during day-to-day activities (less with robotic surgery), and overall physical quality of life (better with robotic surgery).
However these differences did level out by the end of the 12 week period.
"The clinical community waits with anticipation for the 1-year oncological outcomes; the last patient underwent surgery in March, 2015. It will be the interpretation of the longer-term functional and oncological outcomes that reveals the full implications of this study for clinical practice,” said Professor Ara Darzi of Imperial College London.
“Equivalence and non-inferiority should also be seen as positive, showing the innovation has preserved the intended and well established purpose of surgical intervention, such as good oncological outcomes balanced against acceptable functional side-effects.”
The results call into question the cost effectiveness of robotic techniques.
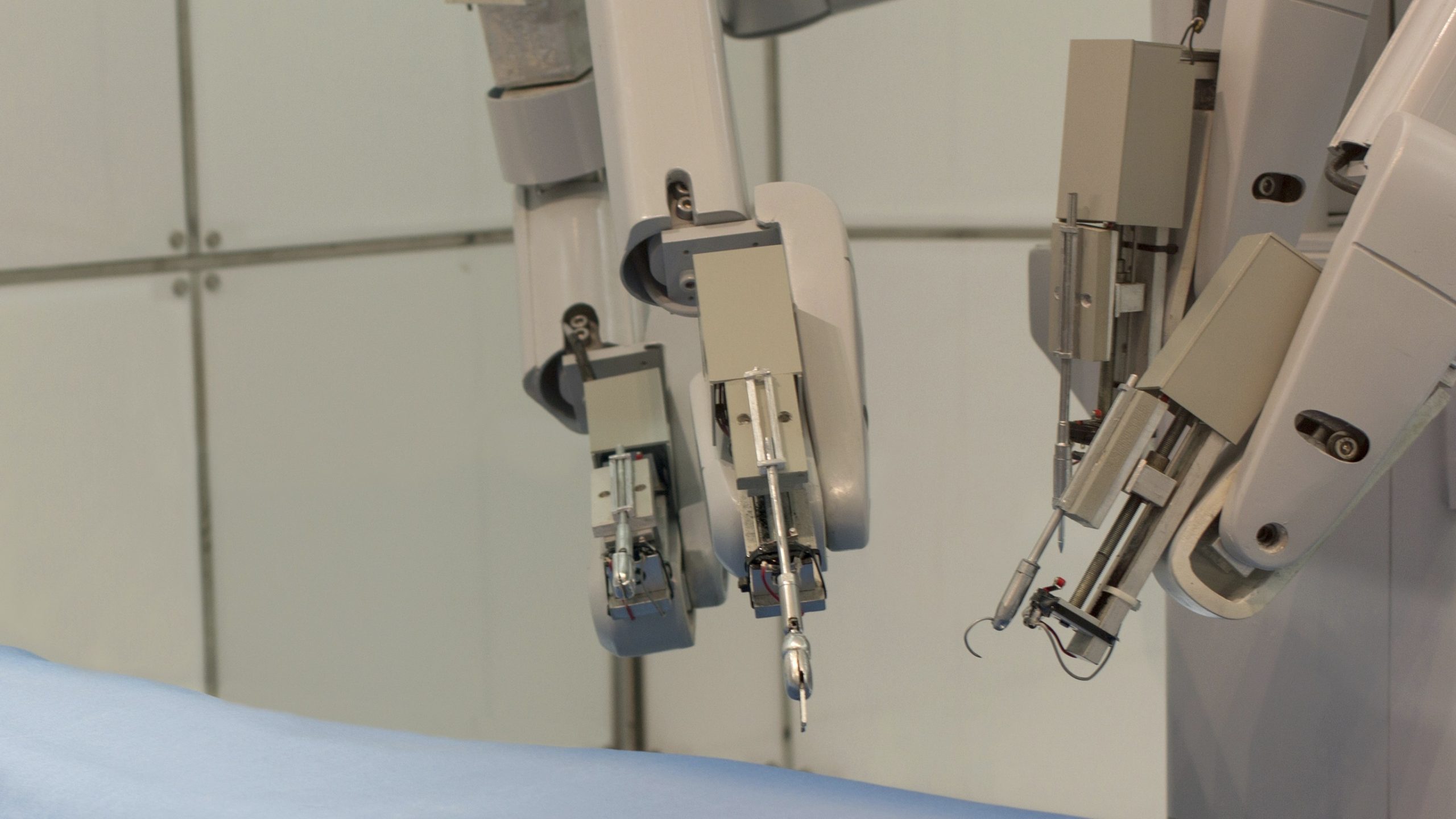
The robots used in robot-assisted laparoscopic prostatectomy (RALP) cost around £1.5 million each making it a much more expensive approach than standard open surgery methods.
The technique is also beginning to be adopted in the treatment of other conditions including cardiothoracic, head and neck, and general surgery.
Longer-term outcomes such as cancer survival will be available upon completion of the study and factors such as urinary and sexual function can continue to improve up to three years post-operation which could highlight more significant differences between the techniques at a later point.











