Merck & Co pens $340m pain drug deal with KCL and Wellcome
Merck & Co has announced a deal with King’s College London (KCL) and Wellcome to investigate a new class of painkillers that could provide an alternative to opioids and their dangerous side-effects.
Known as MSD outside of the US, the big pharma has signed a collaborative licence deal with KCL to investigate a class of drugs that blocks a protein known as HCN2, which has been shown to play a role in chronic pain.
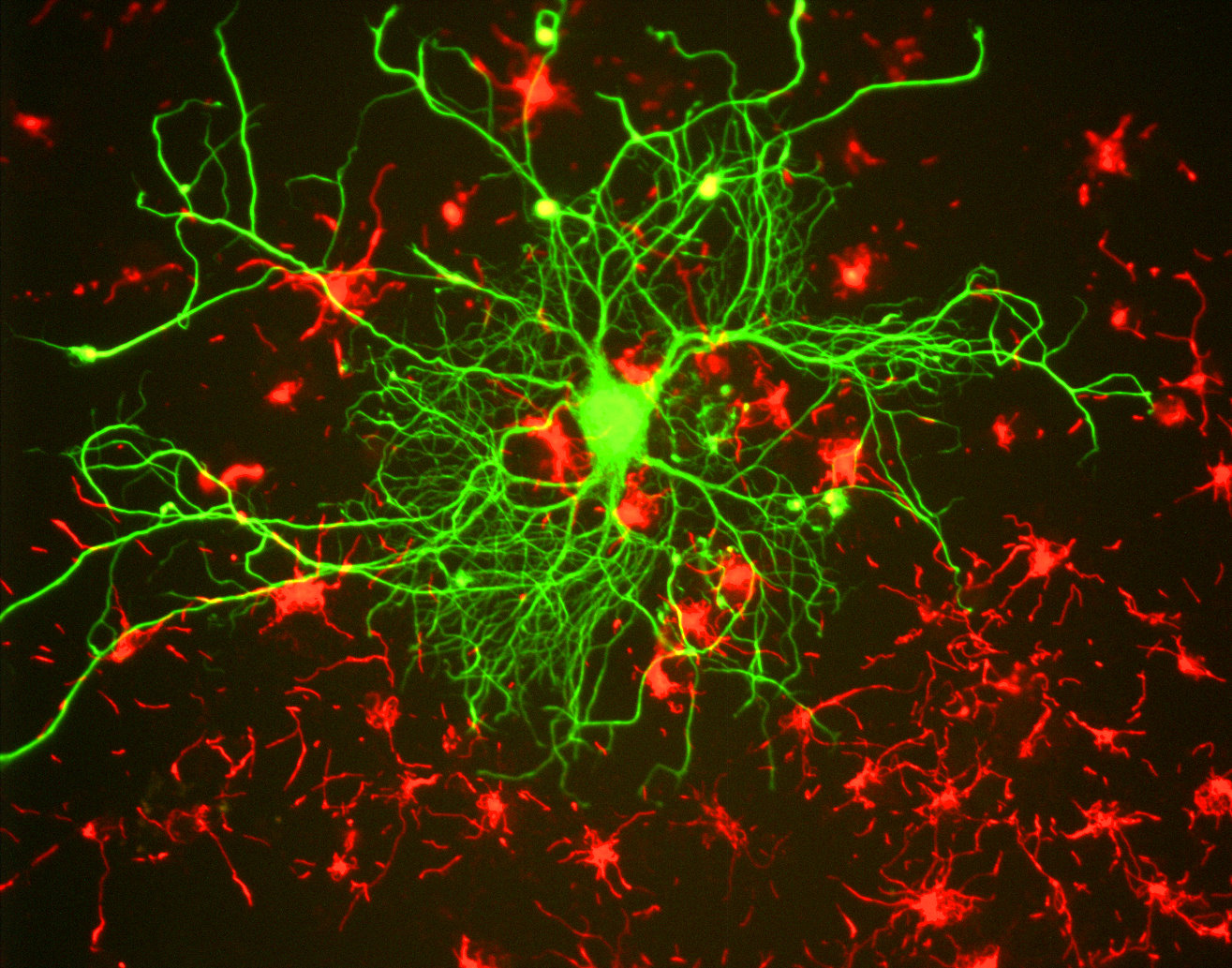
HCN2 can cause a continuous sensation of pain when electrical signals are passed through pain-sensitive nerve fibre.
Research conducted at KCL shows that blocking activity of HCN2 in animal models can deliver effective pain relief without side effects.
The deal is made possible through the work of Professor Peter McNaughton from the Institute of Psychiatry, Psychology and Neuroscience at King’s.
King’s IP and Licensing team and the Wellcome's Innovations team have negotiated a deal with Merck where they are eligible to receive up to $340 million (£263 million) in development and sales milestones, as well as royalties if a drug comes to market.
MSD will also fund further research at McNaughton’s lab into the biological mechanisms of pain.

Dr Peter McNaughton
Since 2012, Wellcome has provided £4.5m in funding to develop Professor McNaughton’s work towards candidate drug compounds for blocking HCN2.
Finding alternatives for highly addictive opioids has become a priority for the FDA, and some pharma companies in the light of the opioid addiction crisis that is gripping America.
Over-prescription of opioids has been blamed for hundreds of thousands of deaths attributed to this type of drug.
After years of delays because of the FDA’s concerns over safety, Pfizer and Eli Lilly are developing the anti-nerve growth factor (NGF) drug tanezumab for conditions such as chronic lower back pain.
Although the drug has hit endpoints in pain relief, there are lingering doubts over its long-term safety.
Results from an osteoarthritis study announced in late January showed that in a small percentage of patients the drug seemed to make the disease become more aggressive, although the drug met its efficacy endpoints at a higher dose.












