Long-term CAR-T data dazzles at ASH
Even though two CAR-T therapies from Gilead and Novartis have been approved in the US, there have been doubts about whether these ‘living drugs’ can continue to produce benefits in the long term.
This is mainly because approval has been based on small trials – albeit with some very strong shorter-term responses.
But new data published at this year’s American Society of Hematology (ASH) conference shows that the therapies can produce durable responses in blood cancer.
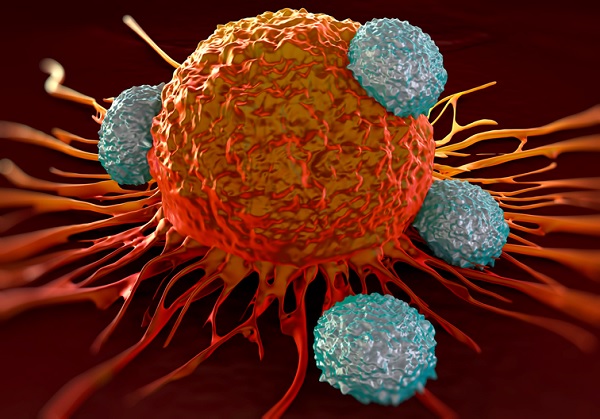
Chimeric antigen receptor T-cell (CAR-T) therapies involve harvesting a patient’s own T-cells, genetically modifying them to attack cancer, then reinjecting them back into the patient.
Gilead produced the longer-term data at ASH, showing that more than half of trial patients with an aggressive form of blood cancer lived for at least a year after a one-time treatment with its CAR-T, Yescarta (axicabtagene ciloleucel).
The ZUMA-1 trial showed after a median period of 15.4 months, 59% of patients with large B-cell lymphoma were still alive, 42% were in remission and 40% had no trace of cancer.
Meanwhile, Novartis also produced six-month data from its rival, Kymriah (tisagenlecleucel) in a group of 81 patients with diffuse large B-cell lymphoma.
Among 46 patients after at least six months of follow-up, 30% had a complete response, with 7% achieving a partial response.
Milestone for CAR-Ts
The New England Journal of Medicine hailed ZUMA-1 as a “milestone” for CAR-T therapies in an editorial.
Authors led by Eric Tran, of the Earle A Chiles Research Institute at the University of Victoria, Oregon, noted that the ZUMA-1 findings validated the centralised cell-manufacturing facility that generates CAR-Ts with a 99% success rate, with patients receiving their cells within 17 days of leukapheresis.
Authors said that “ZUMA-1 provided a blueprint for treating a large number of patients with gene-engineered T-cells”.
But they added that it remains unclear why around half of patients do not have a durable response with CAR-T therapy, which can also cause extreme immune side effects.
While both Kymriah and Yescarta target CD19 antigens, targeting multiple or different B-cell antigens could improve efficacy, they said.
Using the CRISPR-Cas9 gene editing technology to create the CAR-T cells, as opposed to using viral vector technology, may create more potent therapies by more accurately inserting the genes that stimulate the T-cells to attack cancer.
But authors noted the findings reinforce the risks and often serious toxic events observed in earlier trials.
There were three treatment related deaths in ZUMA-1 and one in another smaller trial of Novartis’ rival, they noted.
Cytokine release syndrome, where the immune system goes into overdrive, often causing fever, hypoxia and hypotension, was observed in 93% of patients in ZUMA-1 and 57% of those in the smaller trial of Novartis’ Kymriah.
Future researchers will have to tread carefully, as increasing potency could worsen these toxic effects, authors warned.
“Because the mechanisms of the toxic effects associated with this therapy are not completely understood, strategies that enhance the potency of these products run the risk of inadvertently worsening the already daunting toxic effects,” they said.
Celgene and bluebird bio CAR-T shows promise in myeloma
And bluebird bio also caused a stir at ASH with some strong data from a small trial of its CAR-T bb2121 in advanced multiple myeloma.
All but one of the 18 multiple myeloma patients who had run out of other therapeutic options and then treated with bb2121 responded.
Results showed that 56% remained in remission with a median follow-up of 40 weeks after treatment with bb2121, which is being co-developed by Celgene.
Celgene plans to begin a pivotal trial this month, adding to the race to develop an immunotherapy treatment for myeloma. Last week the FDA lifted the clinical holds on two separate trials combining checkpoint inhibitors (BMS' Opdivo and Roche's Tecentriq) with standard myeloma treatment, dexamethasone and lenalidomide or pomalidomide.












