Gilead and MSD say weekly oral therapy controls HIV
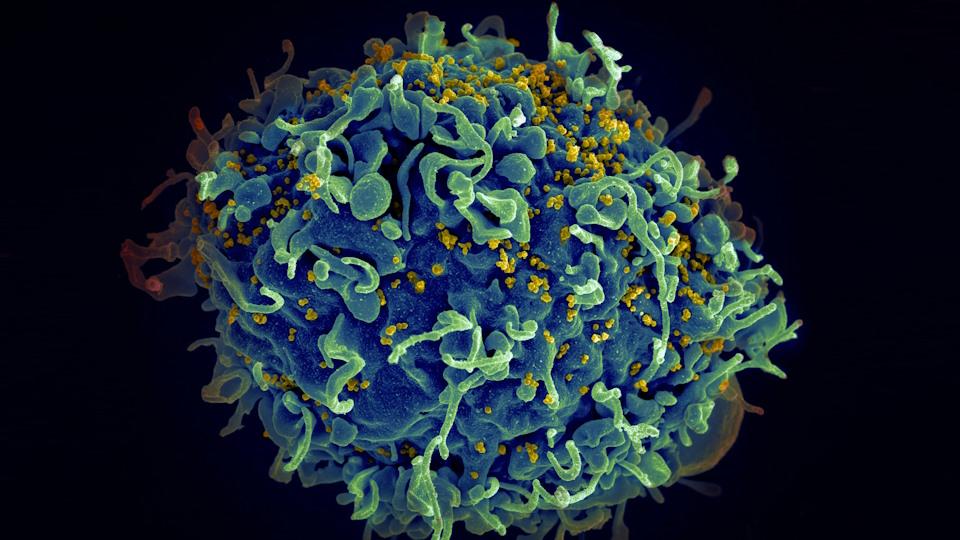
HIV, the AIDS virus (yellow), infecting a human cell
Reducing the burden of treatment for people with HIV has been a key objective for drug developers since antiretroviral therapy (ART) first reached the market. Now, Gilead Sciences and MSD have data on a new combination that provides viral suppression with an oral dose given once a week.
The phase 2 study – reported at the Conference on Retroviruses and Opportunistic Infections (CROI) in Denver, Colorado – looked at the combination of MSD’s experimental long-acting reverse transcriptase inhibitor islatravir with Gilead’s Sunlenca (lenacapavir), a first-in-class capsid inhibitor.
The regimen was compared to daily treatment with Gilead’s best-selling HIV therapy Biktarvy (bictegravir/emtricitabine/tenofovir alafenamide fumarate) in 104 patients whose viral load was already well controlled. After 24 weeks, the weekly treatment maintained a high control rate of 94% viral suppression, compared to 92.3% of the Biktarvy group.
One patient on islatravir/lenacapavir did show a detectable viral load of more than 50 copies/mL at 24 weeks, but fell below that threshold at 30 weeks, according to Gilead and MSD, and two patients discontinued the therapy for reasons that were considered unrelated to the treatment.
While most patients with HIV take daily oral ART to control HIV, injectable products that release drugs over weeks or months have started to reach the market.
That includes Sunlenca, which is approved for resistant HIV as a twice-yearly injection after a lead-in using the oral formulation of the drug used in this study, as well as ViiV Healthcare’s Cabenuva (cabotegravir/rilpivirine), which can be administered every one or two months without lead-in oral dosing.
Islatravir/lenacapavir could provide an additional option for patients reluctant to have injections, but wishing to break free of the daily bind of oral dosing.
“HIV treatment is not one size fits all – developing once-weekly treatment options could help meet the needs of each individual, aiming toward maximising long-term outcomes for people with HIV,” said Gilead’s head of HIV clinical development, Jared Baeten.
Less frequent dosing can address adherence, stigma, and other challenges faced by some individuals taking daily oral ART, said the companies. Failure to stick with regular treatment can allow the virus to bounce back and – at worst – encourage resistance to therapy.
Cabenuva bests daily oral therapy again
There was also news at CROI on Cabenuva, with results from a phase 3 trial showing that once-monthly dosing was better at suppressing viral load than daily oral ART in people who were struggling to adhere to oral ART.
The new data –– from the LATITUDE study sponsored by the National Institute of Allergy and Infectious Disease (NIAID) – follows an earlier trial that showed that Cabenuva was better at suppressing viral load in patients who already have HIV well under control.
Cabenuva is currently approved for virologically suppressed patients who are already on a stable oral ART regimen, with no history of treatment failure, so the new data takes the therapy into a new patient setting.
“It’s estimated that one-third of people living with HIV in the US struggle with maintaining viral suppression,” said ViiV’s head of R&D, Kimberly Smith, who suggested that Cabenuva “could be important for some people in this group, giving them another option to help keep their virus under control and improve their health.”
The main endpoint in LATITUDE – earliest occurrence of virologic failure (VF) or treatment discontinuation – did not meet the predefined stopping criterion at this interim analysis, but was better than standard ART on the secondary endpoints of VF and treatment-related failure. The trial’s data monitoring committee has now recommended that all patients switch to Cabenuva.
Meanwhile, ViiV also presented preliminary phase 1 data on a new ultra-long-acting cabotegravir formulation – called CAB-ULA – that it says could extend the dosing interval to “at least four months.”
Photo by National Cancer Institute on Unsplash













