FDA says no to Checkpoint’s skin cancer drug cosibelimab

Checkpoint Therapeutics' chief executive James Oliviero
Checkpoint Therapeutics’ late entry into the PD-1/PD-L1 inhibitor category, cosibelimab, just got knocked back even further after it was turned down by the FDA as a treatment for skin cancer.
A complete response letter (CRL) from the US regulator cites issues with a third-party contract manufacturer, rather than any safety, efficacy, or labelling issues with the drug, and Checkpoint has said it hopes to re-apply for approval swiftly.
That didn’t stop investors from voting with their feet, and a sell-off drove the Waltham, Massachusetts-based company’s share price down almost 45% in the wake of the announcement.
The scale of the decline may reflect that Checkpoint has been running low on cash as it tries to to get cosibelimab over the line, ending the third quarter with less than $2 million in the bank, although it topped up in October with a $10 million round, which should buy it some time.
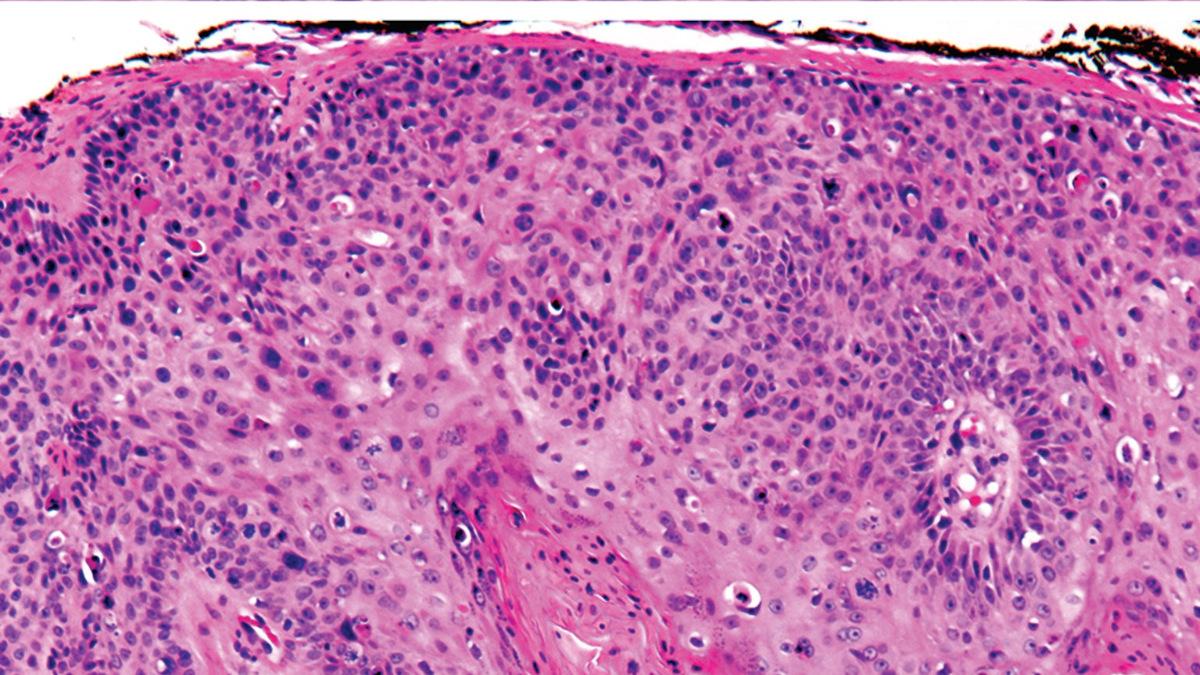
Cosibelimab was filed with the FDA for the treatment of metastatic or locally advanced cutaneous squamous cell carcinoma (cSCC) who are not candidates for curative surgery or radiation, a patient population in which it would compete with well-embedded rivals including MSD’s Keytruda (pembrolizumab) and Regeneron’s Libtayo (cemiplimab), if approved.
Checkpoint has said it may position cosibelimab as a low-cost alternative in the category, backed up by clinical results that suggest its efficacy is at least as good as Keytruda and Libtayo in cSCC.
The US filing was based on clinical trial data that revealed a 55% overall response rate (ORR), including 23% complete responses (CR) in patients with locally advanced cSCC. In those with metastatic disease, the ORR was 50% with 13% CR.
The biotech has said its studies show durability of effect with cosibelimab, which it puts down to a dual mode of action that includes binding to PD-L1 with sustained high target tumour occupancy, driving a T-cell response, and the addition of a functional Fc domain to activate the body’s natural killer (NK) immune cells.
It also says that, unlike PD-1 inhibitors, cosibelimab does not interrupt the body’s PD-1/PD-L2 pathway, which contributes to low rates of autoimmunity – the generation of antibodies that can limit the drug’s effectiveness. The drug was licensed from the Dana-Farber Cancer Institute in 2015.
“As the only deficiencies relate to the FDA’s inspection of our third-party contract manufacturing organisation, we believe we can address the feedback in a resubmission to enable marketing approval in 2024,” said James Oliviero, president and chief executive of Checkpoint.
“We are committed to working closely with our third-party manufacturer and the FDA on our resubmission in order to make cosibelimab available to patients living with cSCC,” he added.
Usually, squamous cell carcinomas are slow-growing and only spread to other parts of the body if they are left untreated for a long time, but in cSCC they can behave more aggressively and spread at a relatively early stage.