Could an antidepressant be used to treat COVID-19?
The antidepressant fluvoxamine merits further investigation as a potential treatment for COVID-19 according to findings of a preliminary trial.
Findings of the trial involving 152 outpatients showed fluvoxamine, a selective serotonin reuptake inhibitor and sigma-1 receptor stopped clinical deterioration compared with placebo.
All the patients on the US-based trial had confirmed COVID-19 and were randomly assigned to receive either fluvoxamine or placebo, three times daily for 15 days.
Participants were community-living, with COVID-19 symptom onset within seven days and oxygen saturation of 92% or greater, according to study findings reported in the Journal of the American Medical Association (JAMA).
Clinical deterioration occurred in no patients in the 80 in the treatment group and six in 72 from the placebo group, although there was a high drop-out rate with only 109 people completing the trial.
The fluvoxamine group had one serious adverse event and 11 other adverse events, whereas the placebo group had six serious adverse events and 12 other adverse events.
Study authors concluded that there was a lower likelihood of clinical deterioration in patients treated with fluvoxamine than those with placebo.
According to study authors, it is the action against the alpha-1 receptor that could be a potential mechanism of action against the virus.
Early studies of COVID-19 found that hospitalisation most often occurs within eight to 10 days of initially mild to moderate symptoms, according to the team from the Washington School of Medicine that conducted the study.
The receptor is linked to regulation of cytokines that cause the inflammation that leads to the serious symptoms seen in some patients with COVID-19.
Previous studies in rats had shown that because of its action on the receptor, fluvoxamine could reduce inflammation and shock.
Authors conceded that if fluvoxamine is determined to be effective in treating COVID-19, the underlying mechanism of action will need further clarification.
Other anti-inflammatory drugs that could show benefits include colchicine and corticosteroids, authors noted.
Perhaps mindful of the many drugs that have failed to live up to early promise in the disease they added that findings were “extremely fragile” because of the small number of endpoint events.
Factors such as distribution of oxygen saturation confounding the results, authors noted.
“The study is limited by a small sample size and short follow-up duration and determination of clinical efficacy would require larger randomised trials with more definitive outcome measures,” they said.
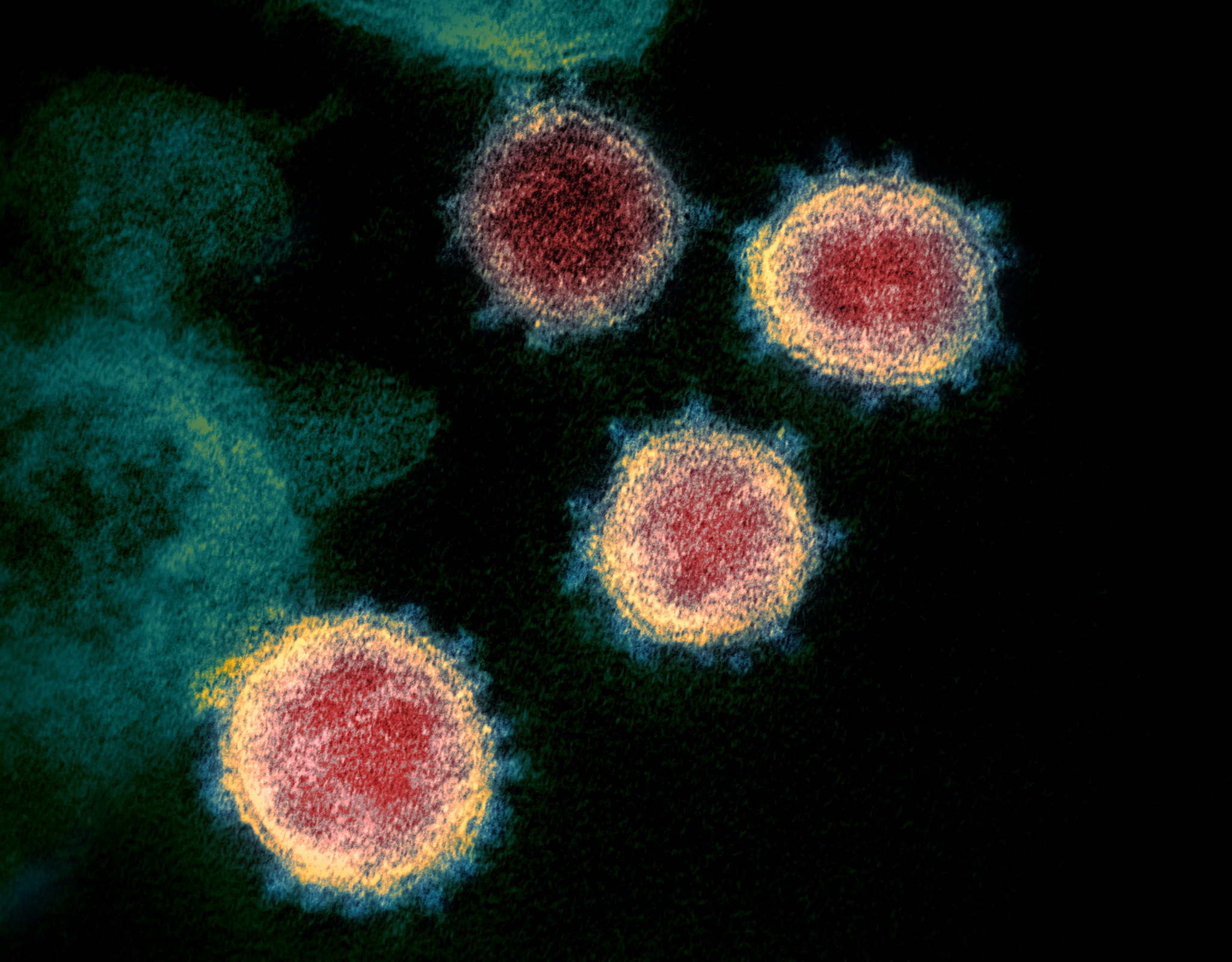
Feature image courtesy of Rocky Mountain Laboratories/NIH












