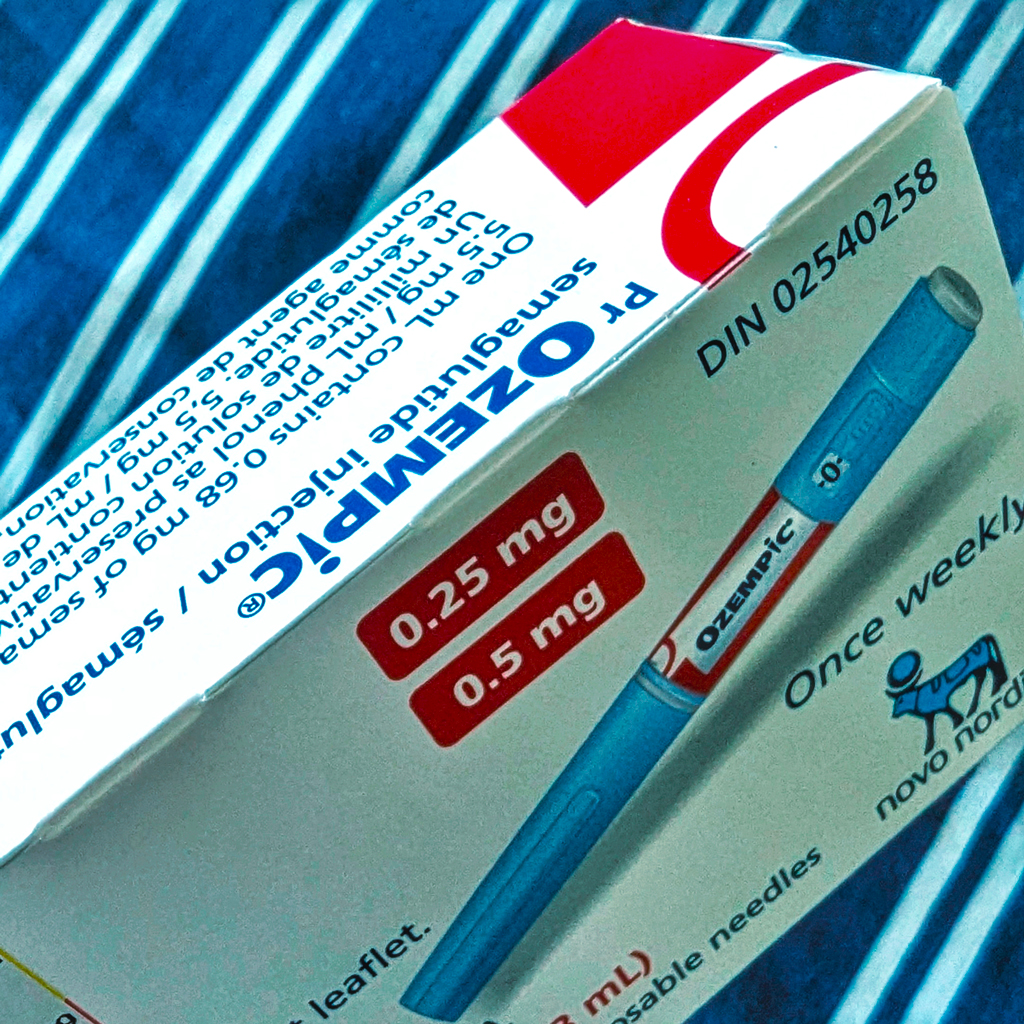
The Ozempic dilemma: Balancing demand, supply, and patient safety in a viral GLP-1 world
As Ozempic and other GLP-1 drugs explode in popularity, driven by their off-label use for rapid weight loss and viral social media trends, the pharmaceutical industry faces unprecedented challenges. With demand far outpacing supply, can manufacturers and regulators keep up with the “trendification” of these treatments – or will patient safety be the cost of their newfound fame?
In the cautious world of healthcare, "going viral" typically raises alarm bells. Yet, for a select few medications, virality can catapult them from mere blockbusters to cultural phenomena. Joining the ranks of Viagra, Xanax, and Botox, a new superstar has emerged: Ozempic.
Ozempic, along with its sister drug Wegovy, belongs to a new class of therapeutic known as GLP-1 receptor agonists. Originally developed for diabetes management, these medications have found a second life as potent weight loss aids. They work by mimicking the action of a hormone called glucagon-like peptide 1 (hence GLP-1), stimulating the body to produce more insulin and decreasing blood sugar spikes by slowing digestion.
With 890 million people affected globally and 42% of American adults classified as obese, the allure of a "miracle" weight loss solution – an average 15% weight reduction, according to clinical research – that reduces your food intake, appetite, and hunger is undeniable.
However, when the realms of beauty and pharma collide, the results can be explosive – and not always in a good way. Ozempic has transcended its medical roots, finding its way into rap lyrics, daytime TV, and even Jimmy Kimmel's Oscars monologue.

This meteoric rise from humble diabetes drug to cultural phenomenon has sent shockwaves through the pharmaceutical supply chain. Despite first gaining FDA approval in 2017, in under three years prescriptions surged 300%, reaching 9 million by September 2023, leaving manufacturers struggling to meet demand.
Indeed, beneath the glitz of Hollywood transformations and viral TikTok challenges lies a darker reality. The “trendification” of Ozempic and semaglutide is putting immense pressure on supply chains and creating a dangerous vacuum – one that's increasingly filled by counterfeit medications, placing countless patients at risk.
Viagra, Xanax, Botox… Ozempic?
The dramatic weight loss of several Hollywood celebrities in recent years sparked whispers of a new secret weapon: Ozempic. Originally a diabetes drug, Ozempic gained a reputation for its off-label ability to trigger significant weight loss. While no celebrity officially endorsed it, the visible transformations of actors, producers, and socialites added fuel to the speculation. When Elon Musk confirmed on Twitter that he was using Wegovy, Ozempic’s sister drug, to achieve his new physique, the secret was out. Hollywood’s latest “miracle drug” was no longer confined to the elite.
Despite its reputation as the “Hollywood weight loss drug”, it’s crucial to note that Ozempic has never been approved for weight management. Only three drugs – Novo Nordisk’s Wegovy and Saxenda, and Eli Lilly’s Zepbound – are actually approved for that purpose. Now, if used correctly, these drugs can be a lifeline for patients. Typically, a responsible doctor approaches prescriptions with a titration mindset: starting at a low dose and slowly increasing it to find the optimal level for each individual patient.
 However, social media paints a very different picture of GLP-1 usage. TikTok, in particular, is flooded with posts promoting rapid, extreme weight loss – sometimes as much as 10 to 15 pounds in a week – by people who do not appear to have a medical need for a weight loss drug. These posts dramatically outnumber those posted by patients using the platform to spread awareness and share experiences, and typically omit critical information about responsible use and potential side effects.
However, social media paints a very different picture of GLP-1 usage. TikTok, in particular, is flooded with posts promoting rapid, extreme weight loss – sometimes as much as 10 to 15 pounds in a week – by people who do not appear to have a medical need for a weight loss drug. These posts dramatically outnumber those posted by patients using the platform to spread awareness and share experiences, and typically omit critical information about responsible use and potential side effects.
Even under prescription guidelines, drugs like Ozempic come with side effects that are extensively studied and regulated. When used without medical supervision, the risks become unpredictable and potentially dangerous. Influencers have amplified this trend, with TikTok becoming the breeding ground for the “Ozempic phenomenon”. Hashtags like #Ozempic and #OzempicJourney have proliferated, transforming the drug into a perceived “quick-fix” for rapid weight loss, divorced from its original medical context.
“It was not expected to happen,” says Tinglong Dai, a public health supply chain expert from Johns Hopkins Carey Business School. “Ozempic serves a relatively niche market for type 2 diabetes patients, but that’s not the reason it’s in shortage now. The surge in demand stems from people discovering its off-label use, turning it into a trend, almost like a fashion statement. Social media accelerated this demand overnight.”
TikTok has indeed turned Ozempic into a lifestyle trend, with over 273 million views on the #Ozempic hashtag alone. Videos range from testimonials of rapid weight loss to viral parodies, like the “Ozempic face” trend, where users joke about the gaunt appearance the drug allegedly gives them. Parodies of the Ozempic jingle and challenges like the “Ozempic hand” test further underscore how the drug has infiltrated popular culture. Once a serious treatment for metabolic conditions, it is now casually discussed alongside fashion and beauty trends.
But this popularity comes with serious risks. The informal and often misleading discourse on platforms like TikTok lacks the critical medical oversight that typically accompanies prescription medications. Social media influencers, often unregulated, showcase examples of rapid weight loss, sometimes using images of individuals who wouldn’t even be classified as obese. As more users seek out Ozempic for weight loss, it has caused widespread shortages, leaving diabetes patients – who rely on the drug for their health – struggling to access it.
Despite the drug’s viral fame, actually obtaining Ozempic is no easy task. The process is not as simple as seeing a TikTok post and getting a prescription; it involves a comprehensive evaluation of the patient’s health and lifestyle. Patients often face significant barriers, with insurance companies employing prior authorisation processes to manage costs and ensure proper use. This can require consultations with obesity specialists or participation in lengthy weight management programmes before a GLP-1 receptor agonist is even considered. Many are discouraged by the high price tag, even with insurance coverage, and some struggle to afford the copays.
Persistent drug shortages add to the complexity, leaving patients unable to fill their prescriptions, even after navigating the insurance maze. These barriers have created a complex landscape wherein demand outstrips supply, fuelling frustration for legitimate patients and encouraging the rise of a dangerous black market for counterfeit drugs.
Shortages and growing demand
The sudden and overwhelming demand for GLP-1 agonists, like Ozempic and Wegovy, has placed immense pressure on pharmaceutical supply chains. What started as a treatment for type 2 diabetes has rapidly expanded into a weight-loss phenomenon, far exceeding the initial market’s scope. According to Dai, the unexpected surge in demand has stretched biomanufacturing capabilities to their limit: “None of these companies could just ramp up their production capacity overnight because that’s not how biomanufacturing works. It takes years to build new facilities, get regulatory approvals, and expand production capacity.”
The core issue isn’t just production; it’s the sheer volume of demand. With approximately 40% of the US population struggling with obesity, the pool of potential GLP-1 users has ballooned far beyond type 2 diabetes patients. “You no longer talk about 5% or 6% of the population; you’re talking about 40%,” says Dai. This unexpected growth has left many diabetes patients in a precarious position, struggling to fill prescriptions, often travelling hundreds of miles in search of the drug.
Pharmaceutical companies are now racing to catch up. Eli Lilly has invested $5.3 billion to expand manufacturing capacity, while Novo Nordisk is building a $4.1 billion fill-finish plant in Clayton, North Carolina. However, these expansions take time, with Dai noting, “It can easily take two to three years to complete the validation process, get all the paperwork, and get your plants inspected. You won’t be able to start production as early as 2026.”
The complexities of biomanufacturing are a significant hurdle. Precise control over temperature, contamination prevention, and compliance with regulatory standards make scaling up production a lengthy process. “You need a lot of workers, testing, retesting, and maintaining conditions to ensure safety. It’s a very tricky process,” Dai emphasises.
As pharmaceutical companies work to scale up production, they must also manage patient expectations. Healthcare providers have been advised to limit new prescriptions, and off-label use has been discouraged. “The best thing they can do is lower everyone’s expectations, while they spend billions of dollars to increase production,” says Dai.
With significant investments underway and new entrants like Sanofi and AstraZeneca considering the market, there is optimism that supply will eventually meet demand. However - as Dai cautions - “everything that goes up must eventually come down”, hinting that the current frenzy around GLP-1s may subside, leaving manufacturers to strike a careful balance between production and demand.
Exploiting a growing appetite for weight loss drugs
The soaring demand for weight loss drugs, coupled with global supply shortages, has created a perfect storm for a more insidious problem to thrive: a flourishing counterfeit market that preys on desperate patients. As shortages persist and demand skyrockets, illicit sellers are stepping in, offering fake or substandard versions of these drugs to patients seeking affordable alternatives. This trend is particularly noticeable online, where unregulated websites and social media ads peddle counterfeit versions of popular weight loss medications, often with enticing discount codes.
Tim Mackey, a professor at UC San Diego who has conducted research into no-prescription GLP-1 purchases online, notes: "Whenever a drug becomes popular, it's going to be available illegally online." Indeed, Mackey’s research uncovered over 1,000 links related to illegal sales of semaglutide, with 42% belonging to 59 illegal online pharmacy sites. These sites often masquerade as research chemical vendors or tout the drugs as "pharmaceutical grade" or "not for human consumption", without requiring a prescription. According to Mackey, "Even though they're representing themselves as research chemical providers, they're actually very directly selling into the human patient market."
The issue has caught the attention of global regulators, who have issued warnings about counterfeit semaglutides. In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) reported seizing 369 potentially fake Ozempic pens between January and October in 2023, marking the first identification of such counterfeits in the country. The United States FDA has seized thousands of counterfeit Ozempic units and, in June 2024, the World Health Organization (WHO) issued a medical product alert regarding falsified batches of semaglutide products, specifically Ozempic, detected in Brazil, the UK, and the US.
The counterfeit operation extends beyond mere imitation. Criminals are using forged drug batch numbers to sell dangerous lookalike weight loss products, potentially linked to a massive global counterfeiting operation. Pharmaceutical companies authenticate batches of drugs with combinations of letters and numbers printed on the packaging, which are then used to track the product in a given country. However, criminals can obtain these batch numbers through corrupt connections at manufacturing facilities or by purchasing genuine drugs and using scanning technology to copy the packaging.
The health risks posed by counterfeit drugs are severe. Regulatory bodies worldwide have reported incidents of severe side effects linked to fake semaglutide products, including hypoglycaemia and seizures. In Austria, patients experienced life-threatening symptoms after using falsified Ozempic, while in Lebanon 11 people suffered dangerously low blood sugar after injecting suspected counterfeit versions.
The problem extends beyond just drug quality. Mackey's team found that many illegal sellers engage in non-delivery schemes or scams, including hidden charges, such as fake customs fees. In one instance, they were asked for an additional $1,000 to clear supposed customs fees, which was later confirmed to be a scam.
As the demand for GLP-1 drugs continues to rise and access remains limited, the proliferation of counterfeit products is likely to persist. As Mackey warns: "It's just the beginning of a long process where we're going to have counterfeit GLP-1s on the web, and it's not going to be something we solve very quickly."
The weight of deception
Regulators and law enforcement are hard at work in the pursuit and closure of these black market sites. But there is one big problem, particularly in the online world. Fake websites are like a hydra: shut down one bad actor and two more will appear in its place. As such, it is an ongoing uphill battle for industry and regulators to counter this trend.
As TikTok tightens its guidelines and pharmaceutical companies race to address supply issues, a larger question looms: are manufacturers truly prepared to navigate the combined forces of social media-driven demand and regulatory loopholes in the pharmaceutical market?
The ongoing battle against counterfeit GLP-1 drugs and supply shortages highlights the complex challenges faced by companies like Novo Nordisk and Eli Lilly. Despite proactive measures, including legal actions and increased security efforts, the problem persists. Moreover, the 503B programme's regulatory fragmentation further complicates matters, allowing seemingly “trustworthy” direct-to-consumer companies to capitalise on compounded semaglutide sales, with far less stringent oversight than their name brand inspiration.
Meanwhile, as influencers on social media platforms like TikTok continue to fuel the narrative of these drugs as "miracle" weight-loss solutions, transforming treatments for serious metabolic diseases into fashionable weight-loss solutions, despite manufacturers' attempts to promote responsible use; the industry has been left to grapple with the short- and long-term consequences of this multifaceted and rapidly evolving landscape.
About the author
Eloise McLennan is the editor for pharmaphorum’s Deep Dive magazine. She has been a journalist and editor in the healthcare field for more than five years and has worked at several leading publications in the UK.
Supercharge your pharma insights: Sign up to pharmaphorum's newsletter for daily updates, weekly roundups, and in-depth analysis across all industry sectors.
Want to go deeper?
Continue your journey with these related reads from across pharmaphorum
Click on either of the images below for more articles from this edition of Deep Dive: Commercialisation 2024