Pre-exposure treatment to help prevent HIV
Wider use of Pre-Exposure Prophylaxis (PrEP), where people who don't have HIV take a pill every day, could prevent around 7,400 new HIV infections in the UK by 2020. David Rowlands examines the evidence and calls for the NHS to follow France in offering the treatment for most-at-risk populations.
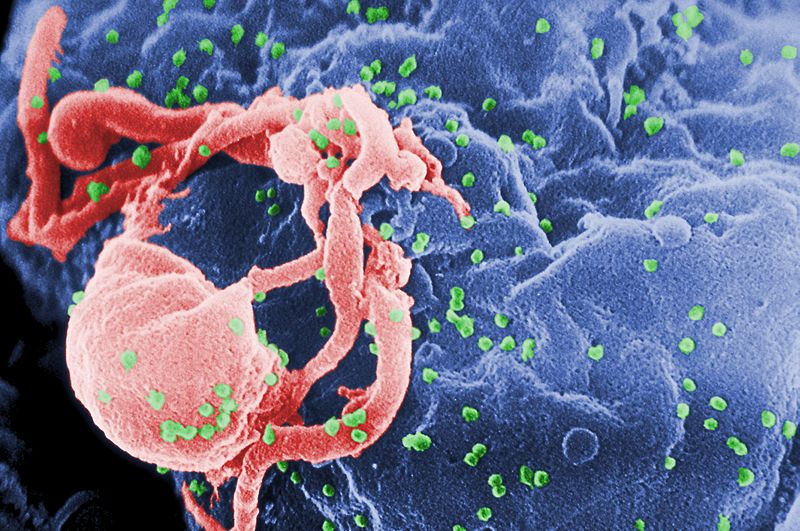
The PrEP pill contains the two medicines tenofovir and emtricitabine, which are also used to treat HIV. For those who are exposed to HIV through sex or injection drug use, PrEP can work to keep the virus from taking hold. Along with other prevention methods, like condoms, PrEP can offer good protection against HIV if taken daily.
Offering PrEP alongside regular HIV testing and early treatment to just a quarter of men who have sex with men (MSM) at high risk of contracting the virus could prevent almost half the number of new diagnoses in that period, boosting calls for the method to be provided free on England's NHS.
New modelling research published in The Lancet HIV journal suggests that, between 2014 and 2020, almost 17,000 new HIV infections in MSM will emerge. Researchers estimated that, even when targeted only at high-risk men, PrEP was more effective than all other individual measures aimed at the entire UK MSM population.
Most recent Public Health England figures show an estimated 103,700 people in the UK were living with HIV in 2014, with around 18,100 unaware and at risk of unknowingly passing the virus on to others. Among the MSM group, 6,500 remained unaware of their HIV infection. High levels of transmission in MSM continue, with 3,360 MSM newly diagnosed in 2014 – the largest number ever recorded.
Can anyone use PrEP?
PrEP may be considered for people who are HIV-negative and at substantial risk for HIV infection. This includes anyone who:
· Is in an ongoing relationship with an HIV-infected partner;
· Is not in a mutually-monogamous relationship with a partner who recently tested HIV-negative and is a gay or bisexual man who has had sex without a condom or been diagnosed with a sexually-transmitted infection within the past six months;
· A heterosexual man or woman who does not regularly use condoms when having sex with partners known to be at risk for HIV (e.g. injecting drug users or bisexual male partners of unknown HIV status); or
· Has, within the past six months, injected illicit drugs and shared equipment, or been in a treatment programme for injection drug use;
· For heterosexual couples where one partner has HIV, PrEP is one of several options to protect the uninfected partner during conception and pregnancy.
Combined strategy
However, for sexually active people, no prevention strategy is 100% effective. Therefore, individuals who use PrEP should use it along with other effective HIV prevention strategies. These include:
• Using condoms consistently and correctly;
• Getting HIV testing with your partners;
• Getting STD testing with your partners;
• Choosing less risky sexual behaviours, such as oral sex.
• For those who inject drugs, participating in a drug treatment programme or using sterile drug injection equipment.
What medications are used in PrEP?
The drug Truvada is a combination of the two HIV medications tenofovir and emtricitabine, which works by blocking important pathways that HIV uses to set up an infection. A daily dose of PrEP in the bloodstream can often stop HIV from taking hold and spreading in the body.
Safety
In clinical studies of PrEP some people had early side effects such as an upset stomach or loss of appetite, but these were mild and usually went away within the first month. Some people also had a mild headache.
The PROUD study
This two-year study, which launched in April 2014, is examining the impact of taking PrEP in the context of how often men have sex, how often they use condoms, and whether they get other sexually-transmitted infections.
It recruited volunteers across England, who were placed randomly into one of two groups. One group was given PrEP from the start and the other was due to be given it after 12 months. Both groups have received support to remain HIV negative throughout the study.
In October 2014 an interim analysis of the PROUD study data showed that PrEP was highly protective against HIV for gay men and other MSM at high risk of infection. The PROUD Trial Steering Committee announced that participants on the deferred arm of the study, who had not yet started PrEP, should be offered the opportunity to begin PrEP ahead of schedule.
As a result, the study design was changed and offered all enrolled participants the opportunity to access PrEP. All study participants will be followed up until the study closes in April 2016.
Call to NHS
The NHS 'cannot afford' to ignore the breakthrough of preventing HIV. It is being urged to allow patients access to PrEP, which could save it millions of pounds by dramatically reducing the chances of them contracting HIV.
Some critics of the drug say the daily pill encourages risky sexual behaviour among gay and bisexual men. They point out that delivery of PrEP 'does not fit neatly into the existing health delivery system: it is an intervention for HIV-negative individuals that requires medical expertise and ongoing interaction with the healthcare system'.
The public health system needs to strengthen ties between community-based organisations and sexual health clinics and providers, with a view to adopting ideas such as medical workers delivering PrEP in community settings, as has already been done to some extent with testing. Community-based organisations can assist with publicity and outreach.
PrEP in France
In December 2015 the French Ministry of Health was the first in Europe to authorise access to PrEP for populations most at risk of HIV infection. This decision was largely based on the results of the IPERGAY study.
IPERGAY was the first trial to show that using PrEP around the time of sex offered equivalent protection to the daily-dosing regimen.
PrEP is most effective when the right amount of drug is in the right place at the right time. It is critical to be able to offer people a range of dosing options so that they can choose the usage pattern that best fits their periods of sexual risk.
Polls
Throughout 2016 Design-Redefined.co.uk is running monthly polls focusing on HIV and hepatitis topics. Views of patients, organisations, healthcare providers, physicians, stakeholders and policy makers will be collected via online hosting and social networking sites.
Click here to take part.
About the author:
David Rowlands is the director of Design-Redefined.co.uk, delivering effective healthcare communications to enable people with HIV and/or hepatitis C (HCV) to become better engaged with their treatment and care.
Drawing on his established networks and collaboration with partners, David is able to bring healthcare together, by engaging patients & organisations, healthcare providers, physicians, stakeholders & policy makers.
Contact David via Email: david@design-redefined.co.uk, website: http://www.design-redefined.co.uk , Twitter: @DR_tweetUk
Copyright statement:
This article is for use online at www.pharmaphorum.com only.
Articles may be redistributed in other media and non-commercial publications with consent of the author. Any republication must acknowledge the author with a link back to www.design-redefined.co.uk The author may request compensation for republication of any unauthorised content.
Read more from David Rowlands:











