Digital health round-up: Robot tells MPs that AI could transform elderly care
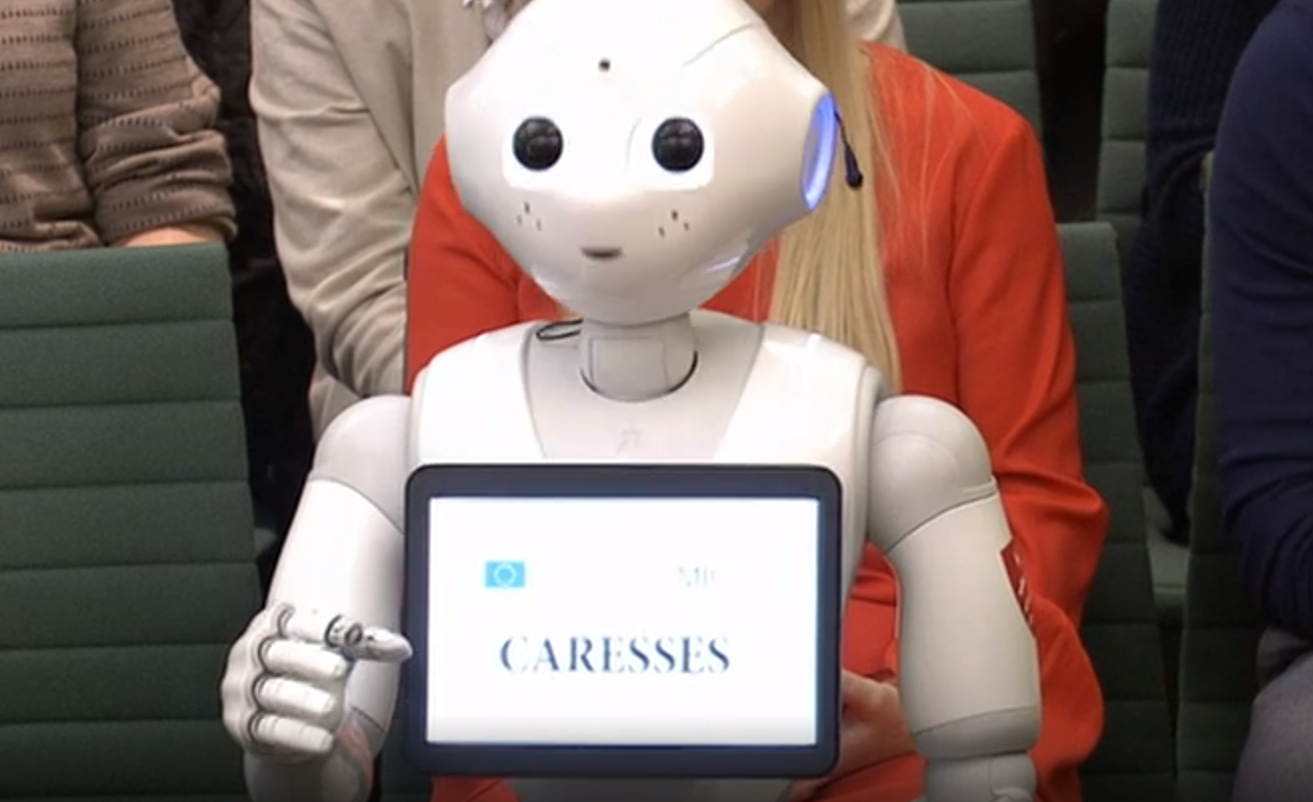
A House of Commons committee questioned a humanoid robot, Pepper, to see how artificial intelligence (AI) and robotics can be used to help care for older people.
Pepper is currently based at Middlesex University and works with final year students on robotics, psychology, biomedicine and education.
An identical robot with different programming is also part of a three-year international research project called Caresses, which is developing the world’s first culturally aware robots aimed at assisting with care for older people.
Pepper told the education select committee that the service could cut costs for caring for older people, as well as helping with issues such as loneliness.
Pepper said: “Assistive intelligent robots for older people could relieve pressure on hospitals and care homes as well as improve the care delivery at home and promote independent living for elderly people.”
SoftBank Robotics, the firm behind Pepper, claims that the humanoid is capable of ‘understanding and reacting to main human emotions’.
It states: “Pepper is well equipped with features and a high level interface for communicating with those around him. Pepper analyses expressions and voice tones using the latest advances in voice recognition.”
Orbita explores voice tech with Brigham and Women’s Hospital
Orbita, a firm specialising in voice and chatbot applications in healthcare, has joined forces with Brigham and Women’s Hospital in Boston, Massachusetts, to explore how voice-enabled and conversational artificial intelligence (AI) can improve patient care.
The organisations will collaborate on innovation of digital health care applications that use voice assistants, chatbots, and other conversational user interfaces to improve patient engagement, remote care, clinical efficiency and business processes.
Orbita will provide its cloud-based platform, Orbita Voice, to enable Brigham’s Digital Innovation Hub to explore, prototype and test the feasibility of voice and chatbot capabilities across a range of inpatient, outpatient and in-home use cases.
Orbita Voice is an enterprise-grade platform for designing, building and maintaining voice and chatbot health care applications that comply with US health regulations, where data security and integrating with existing systems and processes are critical.
Clients include the American Red Cross, Amgen, and the Mayo Clinic.
Brigham and Women’s Health and Orbita began their collaboration through MassChallenge HealthTech, an accelerator based in Massachusetts that matches digital health companies with industry partners to address massive challenges in health.
MassChallenge is a global network of zero-equity start-up accelerators. Headquartered in the US with locations in Boston, Israel, Mexico, Switzerland, Texas, and the UK, MassChallenge drives global innovation by supporting high-potential start-ups across all industries, from anywhere in the world.
Sophia Genetics launches ‘genome browser’ software
The Swiss medical data firm Sophia Genetics has launched the latest iteration of its “genome browser” software, which uses artificial intelligence (AI) to help researchers assess whether errors in the DNA code are leading to diseases such as cancer.
The company is among a growing group of companies offering tools that help scientists to perform complex genetic analyses.
Competitors include BlueBee solutions, Genestack and DNAnexus, which aim to help pharma companies and others analyse genetic information to gain insights that could lead to new therapy approaches.
Sophia’s Alamut Genova is the latest evolution of Alamut Visual, which is already used by over 500 healthcare institutions worldwide.
Its decision support technology enables clinical researchers to solve complex genomic interpretation cases more intuitively.
It graphically displays complex genomic information from various sources and prediction algorithms in a single environment.
Other features include pathology classification, 3D protein visualisation, visualisation of DNA analysis, and new predictions for gene splicing.
The tools on offer allow geneticists to identify and explore variants associated with hereditary disorders and cancer, the company said.
Deep Lens unveils AI pathology assistant
Digital pathology start-up Deep Lens has unveiled an artificial intelligence (AI) platform that will enable pathologists to diagnose cancer patients more swiftly and accurately.
The Ohio-based company has secured early funding worth $3.2m for Virtual Imaging for Pathology Education and Research (VIPER).
The platform uses advanced AI to conduct certain monotonous diagnostic tests instantaneously. This allows diagnoses to be made speedily.
VIPER can also help pathologists to match patients with any relevant clinical trials so that they access the latter as soon as possible.
Another aspect of the platform is to enable pathologists to collaborate with one another and to keep patients informed, and connected with, the most advanced clinical research.
Feedback from hundreds of users based in 65 institutions means VIPER will soon include AI-powered image detection, workflow support, telepathology, cloud storage, and built-in application programming interfaces (APIs) for integration by hardware and software vendors and biopharma companies.
App helps women monitor gestational diabetes

Artificial intelligence company Sensyne Health has launched a new app that helps women manage gestational diabetes, and five NHS hospitals have already signed up.
GDm-Health is a tool enabling remote management of gestational diabetes, reducing the need for expectant mothers to attend additional medical appointments and reducing pressure on midwives and NHS services.
The app, an approved device that complies with requirements in the European Medical Directive, allows patients to connect a blood glucose meter to their smartphone so they can monitor and securely submit real-time information via an app.
Doctors can then review the results outside their usual antenatal appointments.
This frees up clinicians’ time to focus on the woman’s care needs rather than collecting and recording data, meaning they are able to prioritise care for women most at need.
Five NHS Trusts have signed contracts to use GDm-Health and the system will be available to their patients and midwives, following a two-year clinical evaluation in the NHS by over 2,000 women in partnership with Oxford University Hospitals NHS Foundation Trust and Royal Berkshire NHS Foundation Trust.
Three additional NHS Trusts will be implementing GDm-Health in the coming weeks, including Buckinghamshire Healthcare NHS Trust, Croydon Health Services NHS Trust and Milton Keynes University Hospital NHS Foundation Trust.
Gestational diabetes is a pregnancy-related disease that is increasing in prevalence, driven by demographic and lifestyle changes.
In the UK, the rise is predicted to reach a prevalence of over 16%, from a baseline of around 4% in 2008 and is a condition that without tight blood glucose control can lead to adverse maternal and foetal outcomes.
Results published in March 2018 from a randomised controlled trial for GDm-Health (203 participants), demonstrated its value to both women and the NHS including: statistically significant improvement in patient satisfaction, adherence to glucose monitoring, a reduction in caesarean sections, a trend towards reduction in pre-term births and potential for cost-savings to the NHS through improved patient outcomes.












