Healthcare's COVID-19 backlog: how pharma can help

IQVIA's Sarah Rickwood explores how pharma can help healthcare systems address treatment backlogs caused by the COVID-19 pandemic.
As lockdowns started in the West during March 2020, there was, inevitably, much punditry on exit scenarios – for economies, populations, and healthcare systems. Considerable time was devoted to the discussion of V- , U- and L-shaped recoveries.
As we cope with second waves of COVID-19 infections, it is probably fair to say most early pundits were over-optimistic on the length of time the crisis would take to resolve. The pandemic’s aftermath is looking to stretch into the first half of the 2020s. One of the most far reaching impacts will be from the backlog of non-COVID-19 patients who have seen diagnosis and treatment delayed, slowed or even missed and cancelled. For many patients the consequences will be devastating.
With the first wave of lockdowns, treatment backlogs were inevitable due to physical distancing requirements and a pivot to focus on COVID-19. The most immediate impact was cancellation of elective surgeries and other procedures, and the movement of healthcare professional/patient consultations to virtual platforms.
A study in the British Journal of Surgery estimated that globally, 28 million procedures would be cancelled or postponed during the peak 12 weeks of COVID-19 disruption. The same study also made an important prediction: even if all countries increased their normal surgical volume by 20% after the pandemic, it would take a median of 45 weeks to clear the backlog of operations resulting from the 12 weeks of the first wave of disruption.
It is pretty clear that healthcare systems are unlikely to be currently at 120% of their pre-COVID-19 capacity for elective surgeries. In all likelihood, as Europe and the US are in the throes of a second wave of COVID-19 infection, the specific backlog of elective surgery will take longer than predicted to address. Even past the second wave, as vaccines become available, healthcare systems will not return rapidly to pre-pandemic capacities, let alone deliver more than that capacity. The conclusion is that backlog clearance will extend into 2021.
Elective surgery, is, of course at one end of the spectrum of medical conditions with respect to disruptability by the pandemic - by definition they are optional (although if surgeries are postponed, they may become less optional over time), and necessitating visits to a health facility, which may not be possible if there is an infection risk, or that facility has been repurposed for COVID patients. Patients with other conditions, especially cancers, cannot wait.
It is clear that delay in referrals, diagnosis and treatment can mean the difference between treating a cancer that is early stage and therefore often curable to one that is late stage and could result in early death. In an August 2020 paper in the Lancet Oncology, the authors noted that referrals via the 2-week-wait urgent pathway for suspected cancer in England were reported to have decreased by 84%.
The authors used data on cancer patients treated in the English NHS to model the impacts of lockdown induced delays in diagnosis and treatment, and concluded, “Delays in presentation via the 2-week-wait pathway over a 3-month lockdown period (with an average presentational delay of 2 months per patient) would result in 181 additional lives and 3,316 life-years lost as a result of a backlog of referrals of 25%, 361 additional lives and 6,632 life-years lost for a 50% backlog of referrals, and 542 additional lives and 9,948 life-years lost for a 75% backlog in referrals.” The 2-week-wait pathway refers to the request from a General Practitioner in England for an urgent referral to a specialist of a patient exhibiting symptoms which could be cancer.
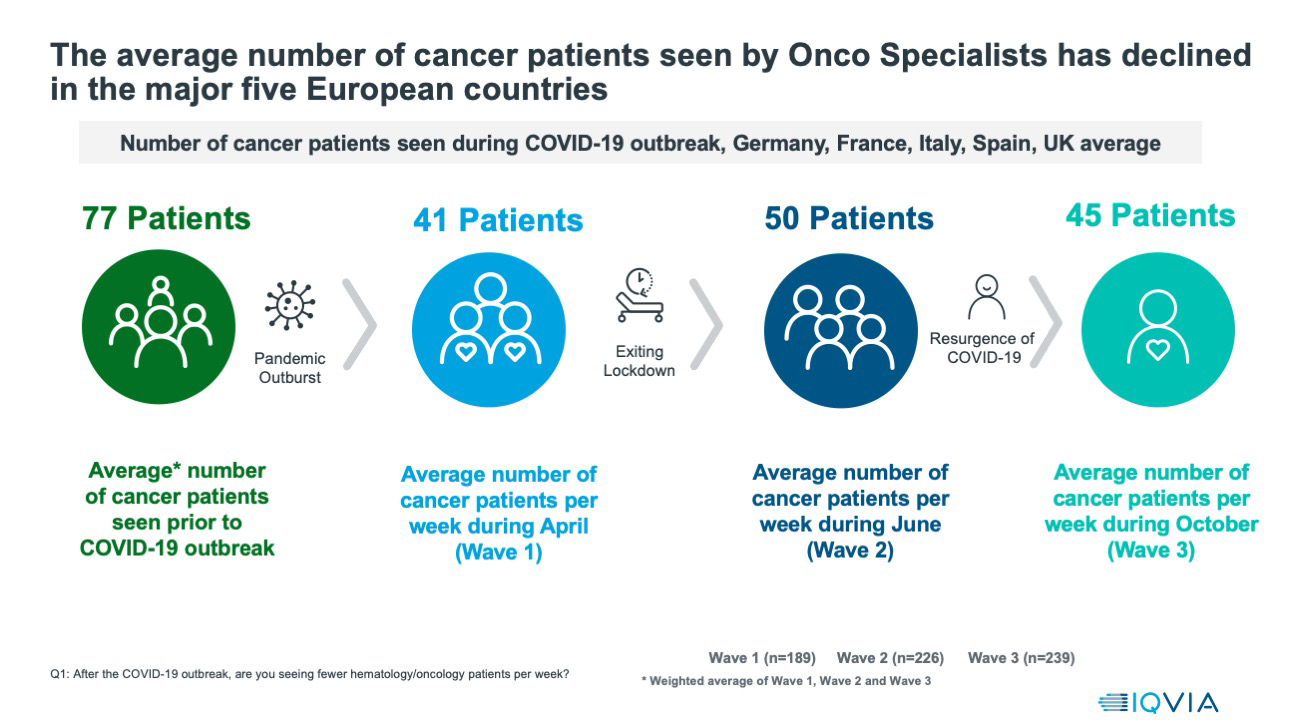
IQVIA has been conducting a survey of oncologists and haematologists on their experience of treating their cancer patients before and during the pandemic. So far, the study has undertaken three waves of research, covering hundreds of oncologists/haematologists across the five major European countries.
The cancer specialists interviewed reported that, on average, they were seeing 77 patients a week prior to the pandemic. This fell to 41 patients a week at the height of the first wave of the pandemic. The June period, which coincided with lows of infection numbers in these countries, was little improved, at 50 patients/week, and as countries faced the second wave of infection in October, the number of patients reported seen per week had fallen back again, to 45. This pattern was seen across the five countries.
Graphic 1
Because of the lockdown, it is not surprising, but very worrying, that cancer specialists reported delays in diagnoses, surgeries and chemotherapy during each of the three waves of interviews. Graphic 2 details the average percentage of specialists reporting each type of delay across the five countries. It is notable that the percentage of specialist reporting delays, which had dropped during the June infection low, rose once again when the second wave was being faced during October.
Graphic 2
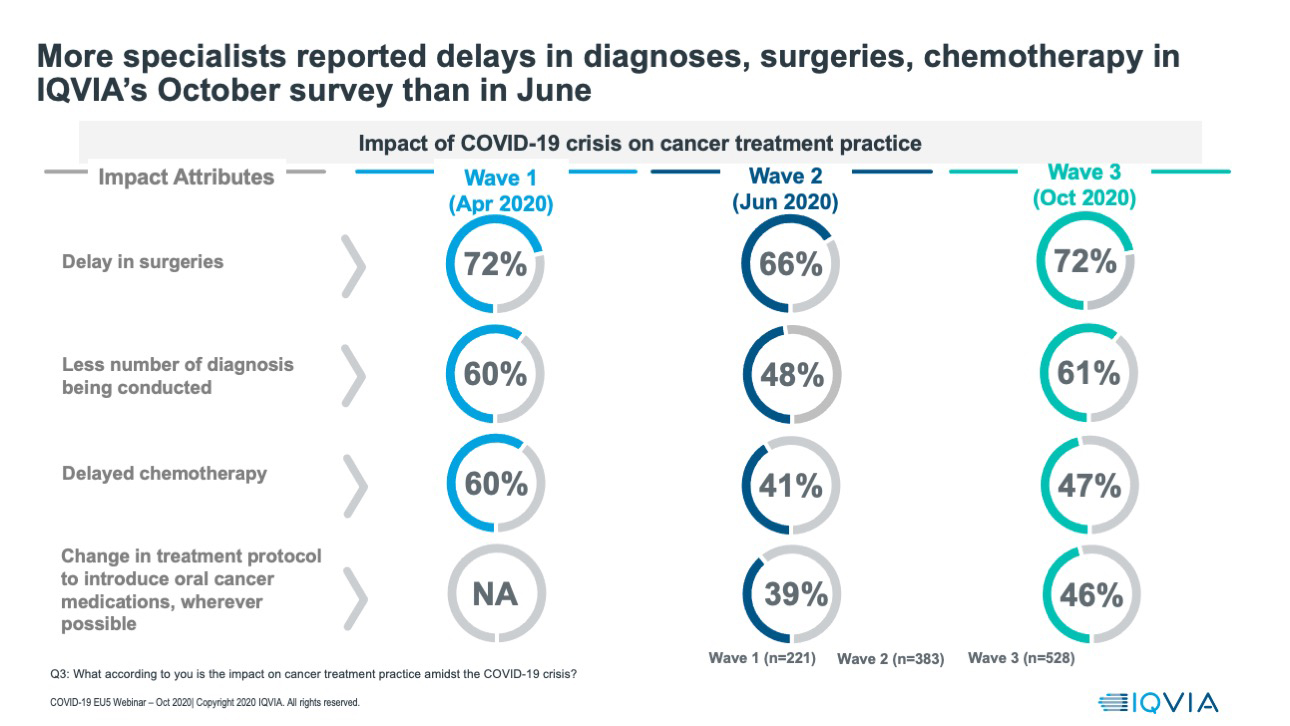
In summary, we have evidence that cancer specialists are reporting delays to patient diagnosis and treatment for cancers across the major five European countries, delays that are continuing past the first waves of the pandemic and into the second, and there are models which suggest that significant increases in mortality and years of life lost will be a consequence of such delays. Treatment backlogs caused by the pandemic are real, will have serious consequences for patients, and will take significant time to resolve.
I’ve picked for discussion two areas, elective surgery and cancer treatment, where patients need to visit health facilities, and in the case of cancers, treatment delays have serious consequences. Not all diseases or conditions are so far along these axes - many chronic conditions can be managed to a very large extent remotely, and for some conditions delays to treatment, even quite lengthy ones, may not have an immediate adverse effect.
Many chronic conditions, such as diabetes, hypertension, dyslipidaemia are also highly prevalent. The impacts of the pandemic backlog on treatment outcomes for these diseases will be played out over years to come, and IQVIA’s longitudinal patient data is already showing decreases in treatment changes (new and switch prescriptions) in relation to key chronic conditions such as diabetes.
The treatment backlog caused by the COVID-19 pandemic matters - to individual patients, to public health systems, and to the pharmaceutical companies developing treatments which patients may now not be receiving as and when they should for optimal treatment. Pharmaceutical companies cannot address this challenge alone. But they can help, and we are starting to see how.
The first step to addressing the backlog is through raising awareness, with health policy makers and with patients. For patients highlighting the importance of seeking treatment, but without generating unnecessary anxiety and health system pressure, is a sensitive task to be done in close collaboration with health systems. Companies need to acknowledge the pressures that healthcare professionals are under and identify where and how they can alleviate pressures and help doctors to help their patients.
Second, as health systems emerge from the pandemic and vaccines are rolled out (and mass vaccinations will also place pressure on health system and some individual doctor’s time), they will need better data and insight on patient journey bottlenecks, on healthcare system capacity stresses and on the services required to remove barriers to effective treatment.
Finally, pharmaceutical companies should play their role in seizing the opportunity to learn and future-proof healthcare delivery against future pandemics. The pandemic highlighted the value of treatments which patients can self-administer, and in many cases there’s been big swings to treatments which can be taken at home - a movement from warfarin, which requires clinic visits, to Direct Oral Anticoagulants (DOACs or NOACs), which do not, for example, in anti-thrombotic treatment. Pharmaceutical companies will undoubtedly place more emphasis on developing treatments that can be home administered and self-administered in the future, and payers and health technology assessors may well value those attributes more highly.
Graphic 3
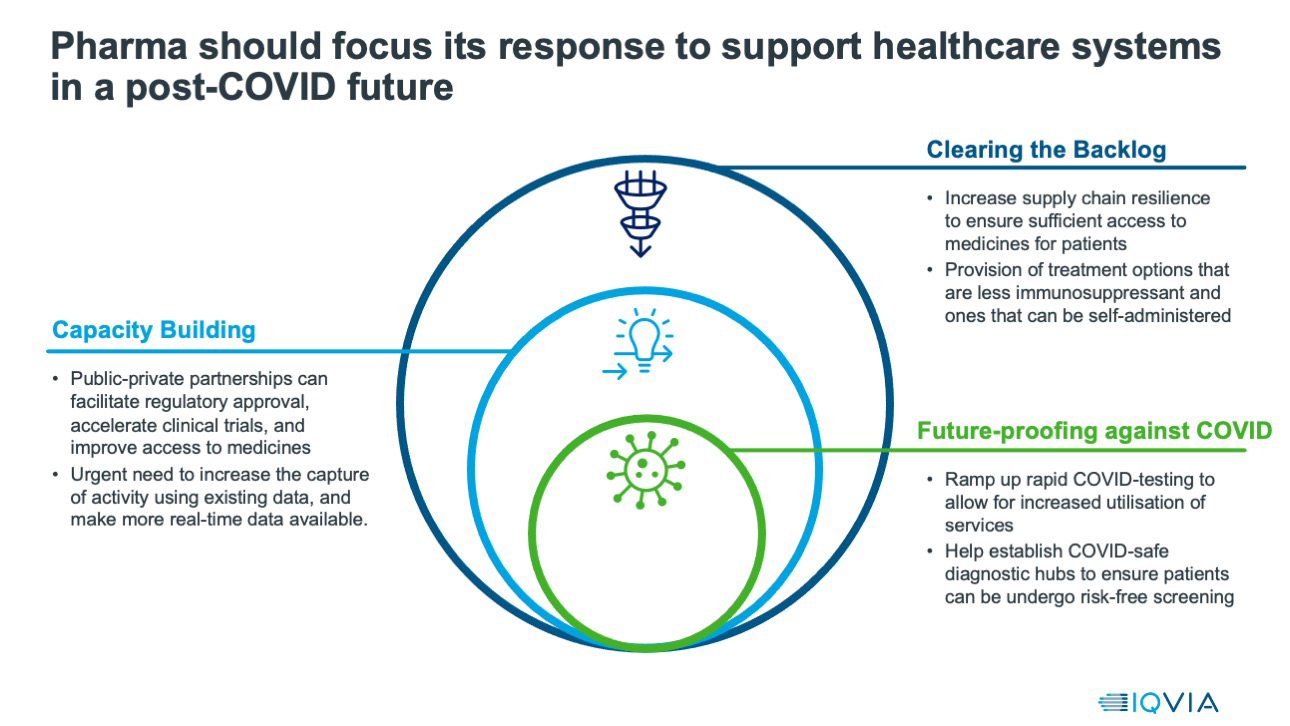
The pharmaceutical industry has risen magnificently to the challenge of COVID-19, in terms of treatment and vaccine development. As the virus is defeated and infection rates fall during 2021, pharma’s next challenge will become increasingly apparent - to help address the other public health crisis of the treatment backlog precipitated by the pandemic. The solutions that pharmaceutical companies can bring to address this, and the relationships that they can forge consequently, will shape the pharmaceutical industry’s role in healthcare systems for the remainder of the 2020s.
About the Author
 Sarah Rickwood has 26 years’ experience as a consultant to the pharmaceutical industry, having worked in Accenture’s pharmaceutical strategy practice prior to joining IQVIA. She has wide experience of international pharmaceutical industry issues, having worked for most of the world’s leading pharmaceutical companies on issues in the US, Europe, Japan and leading emerging markets, and is now vice president, European thought leadership at IQVIA, a team she has run for eight years.
Sarah Rickwood has 26 years’ experience as a consultant to the pharmaceutical industry, having worked in Accenture’s pharmaceutical strategy practice prior to joining IQVIA. She has wide experience of international pharmaceutical industry issues, having worked for most of the world’s leading pharmaceutical companies on issues in the US, Europe, Japan and leading emerging markets, and is now vice president, European thought leadership at IQVIA, a team she has run for eight years.












