Assessing physician practices and expectations in the post-COVID era

The ongoing COVID-19 pandemic has affected the routines of many practicing physicians, including an impact on their prescribing decisions. New research from CRA shows that for many physician practices, prescribing has shifted based on route of administration. These changes, initially presumed to be temporary, may continue beyond the pandemic.
As several COVID-19 vaccine candidates progress to patients and with more than 150 other vaccines in clinical development, global communities look forward to returning to “normal life,” but it is also increasingly likely that what we return to will be a “new normal".
For many practicing physicians, changes presumed to be temporary just a few months ago may in fact become part of more permanent changes to their practice structure. As the COVID-19 pandemic continues, personal protective equipment (PPE) requirements, social distancing, increased telehealth and fewer in-person doctor visits have become common.
Many physicians are also now reporting affordability issues among their patients. In this article, we focus in particular on how COVID-19 may be changing prescribing decisions using market research and claims data.
Together with research partner Dynata, Charles River Associates (CRA) conducted a recent survey of 140 physicians to better understand their perceptions of the pandemic’s effects on their daily practice, including current and potential future changes.
The survey focused on oncologists and neurologists, two specialties that regularly see immunocompromised patients receiving long-term treatment, and also surveyed pulmonologists and urologists to gauge the wider impact on prescribing habits. The findings (both self-reported by physicians and observed in claims) suggest that the pandemic is affecting the therapies that patients receive, as healthcare providers (HCPs) look to reduce the risk of their patients contracting COVID-19.
Analysis of prescribing changes
Based on the survey results, the majority of HCPs (61%), especially oncologists, report changing their prescribing decisions in some way as a result of COVID-19 (see Figure 1). The proportion of physicians who reported changing prescribing decisions varied, ranging from 77% for oncologists to 46% for urologists (pulmonologists and neurologists reported changing their prescribing decisions 54% and 65% of the time, respectively). Ways in which physicians changed their prescribing decisions include:
- Shifting prescribing toward therapies with less frequent dosing (reported most often by oncologists [40%] followed by neurologists [26%])
- Moving toward more established therapies (reported most often by neurologists [37%])
- Moving toward therapies with fewer side effects (reported most often by pulmonologists [26%])
- Most commonly, moving toward therapies that require less in-person contact, such as subcutaneous or oral medicines versus intravenous medicines (reported most often by oncologists [43%] and neurologists [37%])
Figure 1. Changes in Prescribing by Specialty
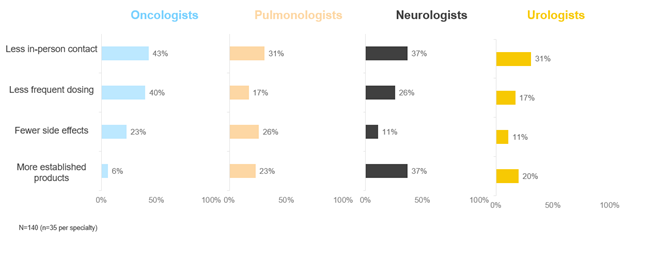
Source: CRA market research (conducted June 2020)
Each of these changes may offer potential benefits for both HCPs and patients. For example, prescribing more established therapies or therapies with more robust efficacy and safety data may make it easier for HCPs to titrate dosing or manage adverse events. Shifting prescribing toward therapies that require less frequent dosing and less in-person contact (such as moving from an intravenous therapy administered in an infusion centre to a subcutaneous therapy that can be administered conveniently at home) has clear potential benefits as a result of reducing interaction that may spread COVID-19.
There are also special considerations for immunocompromised patients including those with cancer or autoimmune disorders such as multiple sclerosis (MS) who are shown to be at increased risk of complications and death from COVID-19. Given their susceptibility to contracting COVID-19 and its associated complications, oncologists and neurologists may be especially motivated to look for opportunities to reduce the risk to immunocompromised patients, including reducing the amount of in-person contact and hands-on management. Switching to therapeutic options that involve less in-person contact may also be more amenable for patients who feel uncomfortable or have difficulty traveling to an infusion centre safely during the pandemic. Fewer patients coming in and out of an infusion centre may help infusion nurses and other staff to also reduce their potential exposure to COVID-19.
Overview of patient claims data
To further explore the impact of COVID-19 on prescribing decisions among neurologists and oncologists specifically, including the proportion of infused therapies prescribed, CRA worked with data from Compile to analyse claims data from patients with MS and HER2+ breast cancer (see Figure 2). These data cover about 30% of US pharmacy claims and about 50% of US medical claims for these conditions.
More than 100,000 MS patients were included in the data set, defined as patients with two or more MS-related medical claims or one or more MS-related medical claims plus a related pharmacy claim identified between January 2019 and June 2020. Focusing on the subset of MS patients shown to have received treatment from neurologists during this time period, infusion therapies (specifically Lemtrada, Ocrevus, and Tysabri) showed a decline of 19% in terms of the total number of claims from February to June 2020.
Our team also reviewed claims data for more than 280,000 HER2+ breast cancer patients during the same observation period (January 2019 to June 2020) and using the same parameters for claims data (two or more HER2+ breast cancer-related medical claims or one or more HER2+ breast cancer-related medical claims plus a related pharmacy claim). Similar to MS patient data, we observed a marked decrease in use of infusion therapies among the subset of HER2+ breast cancer patients shown to have received treatment from oncologists during the observation period. In fact, the claims data suggest that oncologists may be even more likely to shift away from infused therapies to other routes of administration (such as oral or subcutaneous) compared to neurologists. Among HER2+ breast cancer patients in this claims analysis, there was a significant decline of about 41% in terms of the total number of claims using infusion treatment (including Enhertu, Herceptin, Herzuma, Kadcyla, Ogivri, Perjeta, and Trazimera) from oncologists from February to June 2020.
Figure 2. Changes in Prescribing by Specialty
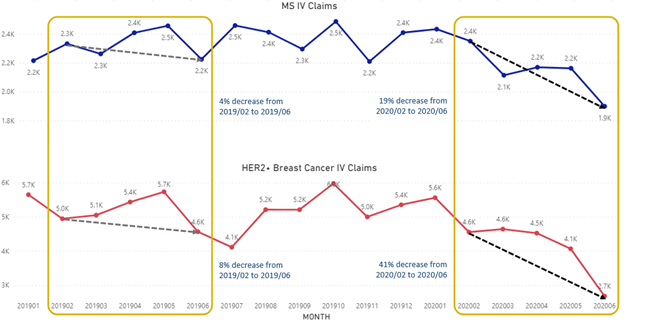
Source: CRA claims data analysis (using claims through June 2020)
Our analysis represents a preliminary review of the impact of COVID-19 on prescribing habits among physicians including specialists. Given the specialised focus in the analysis and the nature of the data, there are caveats associated with using this data source; these may include under-representation of in-patient claims, limited coverage of certain mail-order channels and specialty pharmacies, and the uncertainty of claims capturing for some patient populations.
Impact on patients
Physicians are also adjusting to the impact of COVID-19 on their patients, including patient anxiety and personal finances. More than half of the surveyed physicians in the market research data reported higher patient anxiety due to COVID-19, and most pulmonologists (77%) and oncologists (66%) also reported that patients often contact them with COVID-19-related concerns or questions. They indicate that financial anxiety is likely exacerbating patient anxiety. Many physicians also reported seeing an increase in issues related to financial difficulties among their patients, such as:
- discontinuing or skipping medications due to cost (45% of physicians)
- no longer being able to afford prescribed medications (41% of physicians)
- losing insurance (e.g. through non-employment) (40% of physicians)
- requesting cheaper medications such as generics (35% of physicians)
As the pandemic’s toll on the economy continues, physicians will likely see themselves having more difficult conversations with their patients surrounding medication management and affordability. Being aware of these trends can help physicians prepare their practices to better address such issues. For example, practices may collaborate with pharmaceutical companies to make it easier to help patients find and enroll in financial support programmes.
Taken together, all findings thus far indicate that COVID-19 may be affecting the way physicians prescribe medication and interact with patients, among other impacts. Based on our survey, physicians also cite likely trends such as increased virtual medical conferences and fewer visits with sales representatives, with both outlets possibly becoming less predominant sources of product development information.
In recognition of potential systemic changes in the delivery and access of healthcare services, physicians will continue to adapt their practices to the new environment to address both internal and patient concerns. This may require education from and communication with pharmaceutical companies and other industry stakeholders moving forward. Acknowledging that temporary changes including prescribing changes may become permanent and preparing for this shift can better position HCPs and their practices to succeed in the post-COVID-19 era.
About the authors
Kristen Backor, PhD, is director of the market research Center of Excellence at CRA, providing guidance and oversight for projects concerning customer insights and qualitative and quantitative research assessments.
Eddie Li is director of the Analytics Center of Excellence at CRA, where he specialises in market assessment, promotional response modelling, customer segmentation and patient finding.
Jing Li is a senior associate in the Analytics Center of Excellence at CRA with significant experience in analysis of pharmaceutical claims data.
Elizabeth Rountree is a vice president at CRA with 20+ years of customer insights experience (data analytics, primary market research) in biopharmaceuticals as well as in-depth expertise in neurology and oncology.
Billy Wang is an associate at CRA who has been helping clients define COVID-19 focused strategies since the beginning of the pandemic.
The views expressed herein are the authors’ and not those of Charles River Associates (CRA) or any of the organisations with which the authors are affiliated.












