The gut microbiome: the next breakthrough in cancer?
Ben Hargreaves discovers how research has emerged outlining how the gut microbiome plays a crucial role in patients’ response to cancer treatments. As a result, there are now a number of companies looking to leverage gut microbiota to boost immunotherapies’ potency against cancer.
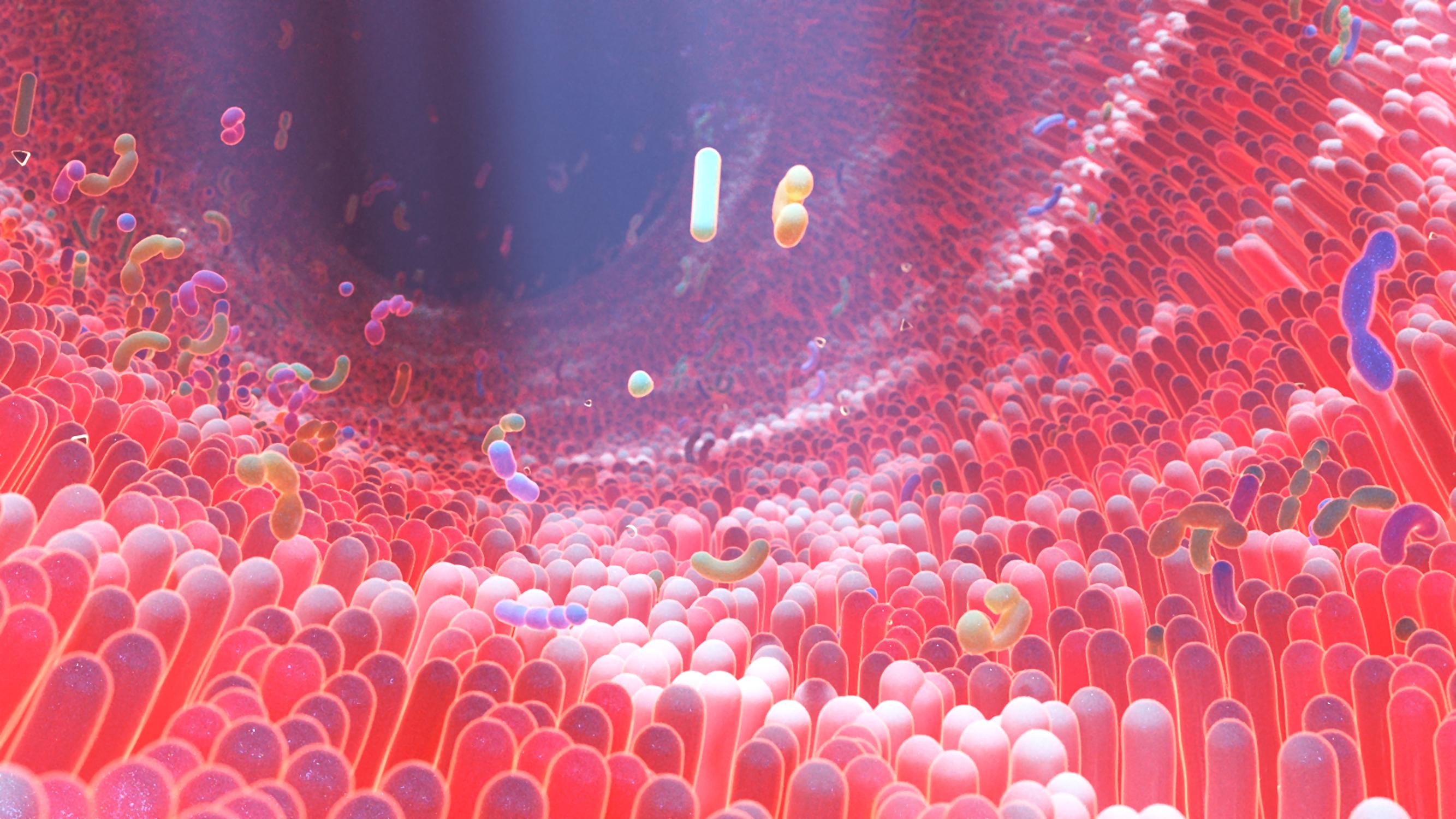
The human microbiome is a complicated system of microbial cells. The number of genes that make up the microbiome is far greater than the number of genes in the cells that make up the human body. Each person’s microbiota contains around 10 to 100 trillion symbiotic microbial cells, which are primarily made up of bacteria in the gut. Scientists are learning to better understand this system, and its impact on our health, thanks to the advances that have occurred in genome sequencing technology. As more has been learned about its influence on human health, the scale of investment into the area has also grown, alongside the number of companies looking to develop therapeutics utilising this knowledge.
With the majority of the human microbiome being made up of bacteria residing in the gut, this has led to a number of potential drug candidates moving through the pipeline targeting the gastrointestinal tract. There is a growing interest in how the microbiome has an impact on the progression of cancer, as well as its ability to make patients more receptive to certain immunotherapies.
Promise in cancer treatment
Research has shown that microbiota can alter cancer susceptibility and progression by modulating inflammation, causing DNA damage, and producing metabolites involved in the formation of cancer cells or tumour suppression. There has also been evidence that gut microbiota can affect the efficiency of chemotherapeutic drugs. Research published in the British Medical Journal shows that altered gut microbiota are associated with resistance to both chemotherapy and immune checkpoint inhibitors, while supplementation with distinct bacterial species can restore responses to anticancer drugs.
As a result, there is now a growing body of biotechs looking at the potential to develop treatments utilising gut microbiota, or to create drugs that target the microbiome to augment the activity of anticancer agents. Pharmaphorum reached out to several biotechs working in the area to learn more about what the promise is for this type of treatment in cancer.
A spokesperson for Enterome, which is a clinical stage company developing immunomodulatory drugs for the treatment of cancer, explained its work in the area: “We have been working to identify and characterise the specific factors that are involved in these responses – by that, we mean bioactive molecules secreted by gut bacteria – with the intention of using that knowledge to create small molecule/short peptide-based immunotherapeutics that follow well understood clinical development and regulatory pathways.”
MaaT Pharma, a biotech focused on restoring and modulating patient-microbiome symbiosis for the treatment of cancer, also spoke with pharmaphorum. A spokesperson for the company explained why the microbiome holds promise for aiding cancer treatment: “Recent studies have shown the key role it plays in educating, regulating, and influencing our immune system, in turn influencing our response to cancer and cancer treatment. In haematology and oncology, the different treatments received by the patients such as chemotherapy, radiotherapy, but also broad-spectrum antibiotics, are creating a state of dysbiosis. This is a sort of vicious circle, and today we do have evidence that you need to correct this dysbiosis to improve the health condition of the patient, but most importantly to improve the efficacy of some well-established treatments.”
Why the interest in immunotherapies
The development of cancer immunotherapies has become one of the key breakthroughs in the treatment of cancer in recent years, particularly immune checkpoint inhibitors. Keytruda (pembrolizumab) has become one of the best-selling treatments on the market, as a PD-L1 inhibitor. The reason for the surge in interest for treatments developed from the microbiome is their capacity to boost the efficacy of such treatments. There has been research showing that the microbiome can stimulate an anti-tumour response by modulating CD8+ T cells, T helper 1, and tumour-associated myeloid cells. The potential was interesting enough for AstraZeneca to agree a collaboration deal with Seres Therapeutics to explore the use of SER-401, an investigational microbiome therapeutic, alongside AZ’s portfolio of anticancer treatments, which includes a checkpoint inhibitor, Imfinzi (durvalumab).
Enterome is developing a type of treatment that it has termed ‘OncoMimics’, which are synthetically manufactured, bacteria-derived peptides that mimic and are cross-reactive with known tumour-associated antigens (TAAs). In terms of what this type of treatment could deliver, the spokesperson explained, “The selection and combination of these peptides into individual immunotherapy candidates is prioritised to engage with a hitherto untapped part of the immune repertoire that exists in every patient: memory T-cells, and redirecting this powerful response against tumours. Importantly, this unique mode of action allows us to overcome the immune tolerance to TAAs, which are recognised as self-antigens, and that severely limits the effectiveness of existing immunotherapies.”
A winning combination?
At this point, Enterome has several of these treatments moving through the clinic, with four drug candidates at the phase 2 stage. The spokesperson stated that some of these trials involve the company’s drug candidate, EO2401, being trialled in combination with the checkpoint inhibitor nivolumab, known by the brand name Opdivo, and bevacizumab, known by the brand name Avastin. The spokesperson added: “EO2401 in combination with nivolumab generated strong systemic immune responses through activation of specific effector memory CD8+ T cells, correlating with clinical efficacy.”
For MaaT Pharma’s part, the company is moving its lead asset, MaaT013, through phase 2a trials in immuno-oncology, and is in phase 3 onco-haematology trials. The treatment is a donor-derived, microbiome ecosystem therapy that contains butycore, a group of bacterial species known to produce anti-inflammatory, short-chain-fatty acids. Similar to Enterome’s drug candidates, MaaT013 is also being explored along with nivolumab, as well as ipilimumab, known by the brand name Yervoy.
“Immune checkpoint inhibitors and other forms of immunotherapy have dramatically improved outcomes for many with cancer, but many patients do not benefit from these treatments. Previous work, including research led by MD Anderson, demonstrates the gut microbiome is a key mediator of individual response to checkpoint inhibitors,” the spokesperson for MaaT Pharma answered, as to why there is such interest in the potential to combine microbiome-targeting therapies with immunotherapies.
Should the combination treatments prove effective, not only could the microbiome treatments improve patient outcomes, but they could also be lucrative for those involved, given the revenues of the treatments involved. If that were to happen, the additional funds should see research into microbiome-targeted therapies accelerate rapidly.