Driving innovation in multiple myeloma to improve the patient experience
Despite being the second most common haematologic cancer globally, treatment options for multiple myeloma remain limited, with a significant need for new therapies.1
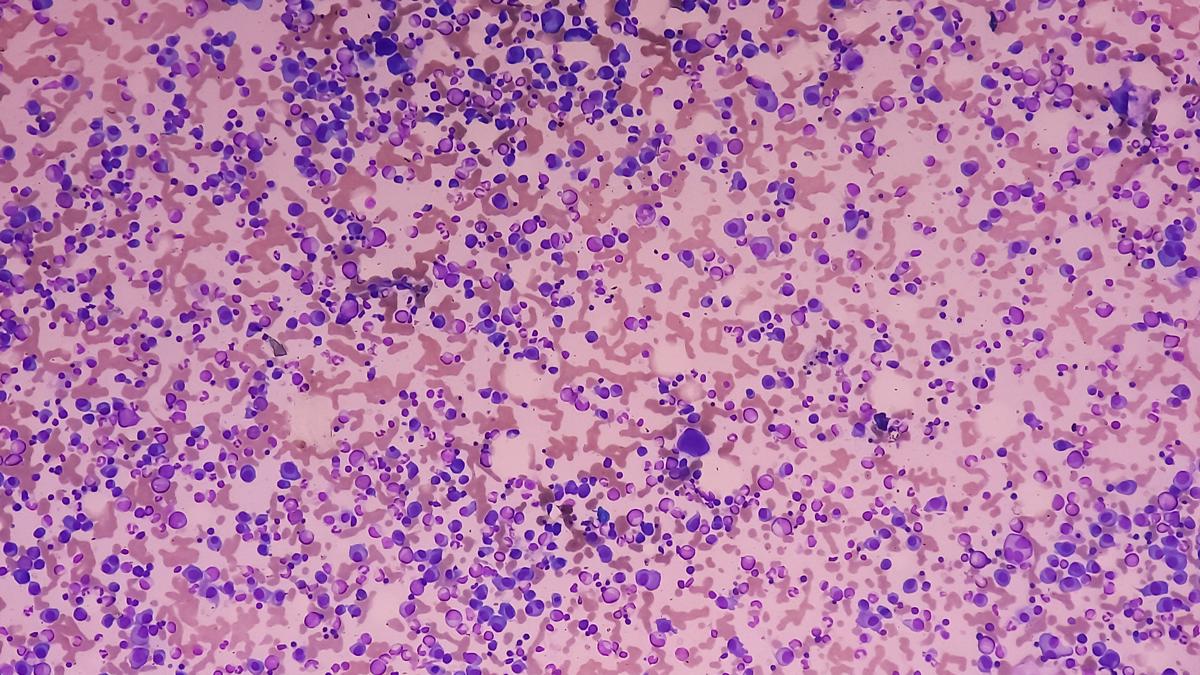
Multiple myeloma originates in blood plasma cells — a type of cell found in bone marrow that is responsible for making antibodies. When these plasma cells become cancerous, they multiply uncontrollably, leading to the overproduction of abnormal proteins that can cause damage to bones, kidneys, and the immune system.2
Today, treatment for multiple myeloma often involves an intensive combination of chemotherapy, steroids, immunomodulatory drugs, and bone marrow transplants to slow down this multiplication and/or eradicate the cancerous cells.3 Sadly, almost all patients who respond to an initial course of treatment eventually relapse and, as the disease progresses, it often becomes refractory.4
Over time, treatments have become more effective at reducing the disease burden of multiple myeloma, but challenges remain. Even when there is no detectable disease, relapse can occur years later, sometimes without warning, and the mechanisms that render the disease incurable are not well understood. Many patients therefore require long-term therapy, resulting in indefinite clinic visits and side effects that are common with prolonged treatment, which ultimately affects their quality of life.1
There is an urgent need for more effective therapies that offer a shorter duration of treatment and enhanced tolerability, to improve outcomes and lessen the burden on patients.
Recent advances with innovative modalities
Despite these challenges, advances in the field are improving the outlook for people diagnosed with multiple myeloma. As evidence, the five-year overall survival rate in the United States has doubled from the 1990s to 2020.5
A deeper understanding of disease biology is identifying new vulnerabilities that can be exploited therapeutically. The emergence of modalities like antibody-drug conjugates (ADCs) and chimeric antigen receptor T-cell (CAR-T) therapies hold great potential for delivering more individualised treatment options across all stages of disease and could shorten treatment duration.6
ADCs combine the precise targeting of monoclonal antibodies and the potency of chemotherapies to selectively kill cancer cells while minimising damage to healthy cells.6 The use of ADCs offers a more precise and better tolerated alternative to chemotherapy, and has the potential to redefine the treatment landscape, especially for patients whose disease has become resistant to other therapies.
CAR-T therapy is already providing longer remission periods for some patients and can even potentially drive cures for certain types of blood cancers, like lymphoma.6-8 CAR-T therapies are a type of living drug that is created by collecting a patient’s T-cells and genetically modifying them so they can seek out and aim to eliminate cancerous cells. In recent clinical trials, CAR-T cell therapies have shown significant efficacy in patients with relapsed/refractory multiple myeloma, offering a new potential treatment for those who have exhausted other options.6
At AstraZeneca, by way of example, we’re exploring strategies to address the needs of as many people living with multiple myeloma as possible; spanning varied fitness levels, treatment settings and backgrounds, and across all stages of disease, to hopefully drive deeper remissions and even cures. Above all, we are working to develop new ways to reduce the treatment burden so patients can maintain the highest quality of life possible.
It’s clear that one size won’t fit all and it’s imperative to develop different therapies so doctors can select the most suitable treatment option for each patient, with the ultimate goal of helping them become disease, therapy, and symptom free.
Looking ahead at challenges, research, and improvements for patients
As the field advances, there are obstacles to overcome. For example, current cell therapy approaches focus on autologous CAR-Ts where scalability, lengthy manufacturing timelines and a need for a specialised infrastructure limit accessibility. Patients must participate in a logistically complicated treatment plan, including waiting for an available treatment slot, travelling to a specialised centre and enduring additional cycles of chemotherapy while they await the production of their CAR-T. We must continue to drive innovations in manufacturing and off-the-shelf allogeneic therapies to address this and bring the potential of cell therapy to more patients.9
Beyond innovative modalities, the use of blood-based monitoring to detect minimal residual disease, which refers to the small number of cancer cells that remain in the body following treatment, is emerging as a promising tool in haematology.10 While the haematology community is still learning how best to apply this in clinical trials, it’s clear this will become an important measure of efficacy, with the potential to transform decision-making in the clinic and enable earlier diagnosis and intervention to ultimately improve patient outcomes.
Although multiple myeloma currently remains an incurable disease, ongoing research and innovation offer hope for improving survival rates and quality of life.1 We are getting closer to potential developments that will hopefully mark a shift in how multiple myeloma can be treated, with the potential for more individualised, precise, and durable strategies. With these goals and the development of new treatments, we hope to revolutionise care for all those living with multiple myeloma across the world and move closer to cures.
References
- Dima D, Jiang D, Singh DJ, et al. Multiple Myeloma Therapy: Emerging Trends and Challenges. Cancers (Basel). 2022 Aug 23;14(17):4082.
- American Cancer Society. What Is Multiple Myeloma? Last accessed October 2024. Available at: https://www.cancer.org/cancer/types/multiple-myeloma/about/what-is-multiple-myeloma.html
- Treatment Options for Multiple Myeloma and Other Plasma Cell Disorders. Last accessed October 2024. Available at: https://www.cancer.org/cancer/types/multiple-myeloma/treating/by-stage.html
- Leukemia & Lymphoma Society. Refractory and Relapsed. Last accessed October 2024. Available at: https://www.lls.org/myeloma/treatment/refractory-and-relapsed
- Zhu DT, Park A, Lai A. et al. Multiple myeloma incidence and mortality trends in the United States, 1999–2020. Sci Rep. 2024; 14:14564.
- Sammartano V, Franceschini M, Fredducci S, et al. Anti-BCMA novel therapies for multiple myeloma. Cancer Drug Resist. 2023 Mar 22;6(1):169-181
- US FDA. FDA D.I.S.C.O. Burst Edition: FDA approval of CARVYKTI (ciltacabtagene autoleucel) for the treatment of adult patients with relapsed or refractory multiple myeloma after four or more prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. Last accessed October 2024. Available at: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-disco-burst-edition-fda-approval-carvykti-ciltacabtagene-autoleucel-treatment-adult-patients.
- National Cancer Institute. Trial Confirms CAR T-Cell Therapy Benefits People with Aggressive Lymphomas. Last accessed October 2024. Available at: https://www.cancer.gov/news-events/cancer-currents-blog/2023/large-b-cell-lymphoma-axi-cel-zuma-7-trial.
- Rendo MJ, Joseph JJ, Phan LM, DeStefano CB. CAR T-Cell Therapy for Patients with Multiple Myeloma: Current Evidence and Challenges. Blood Lymphat Cancer. 2022 Aug 29;12:119-136.
- Leukemia & Lymphoma Society. Minimal Residual Disease (MRD). Last accessed October 2024. Available at: https://www.lls.org/sites/default/files/National/USA/Pdf/Publications/FS35_MRD_Final_2019.pdf












