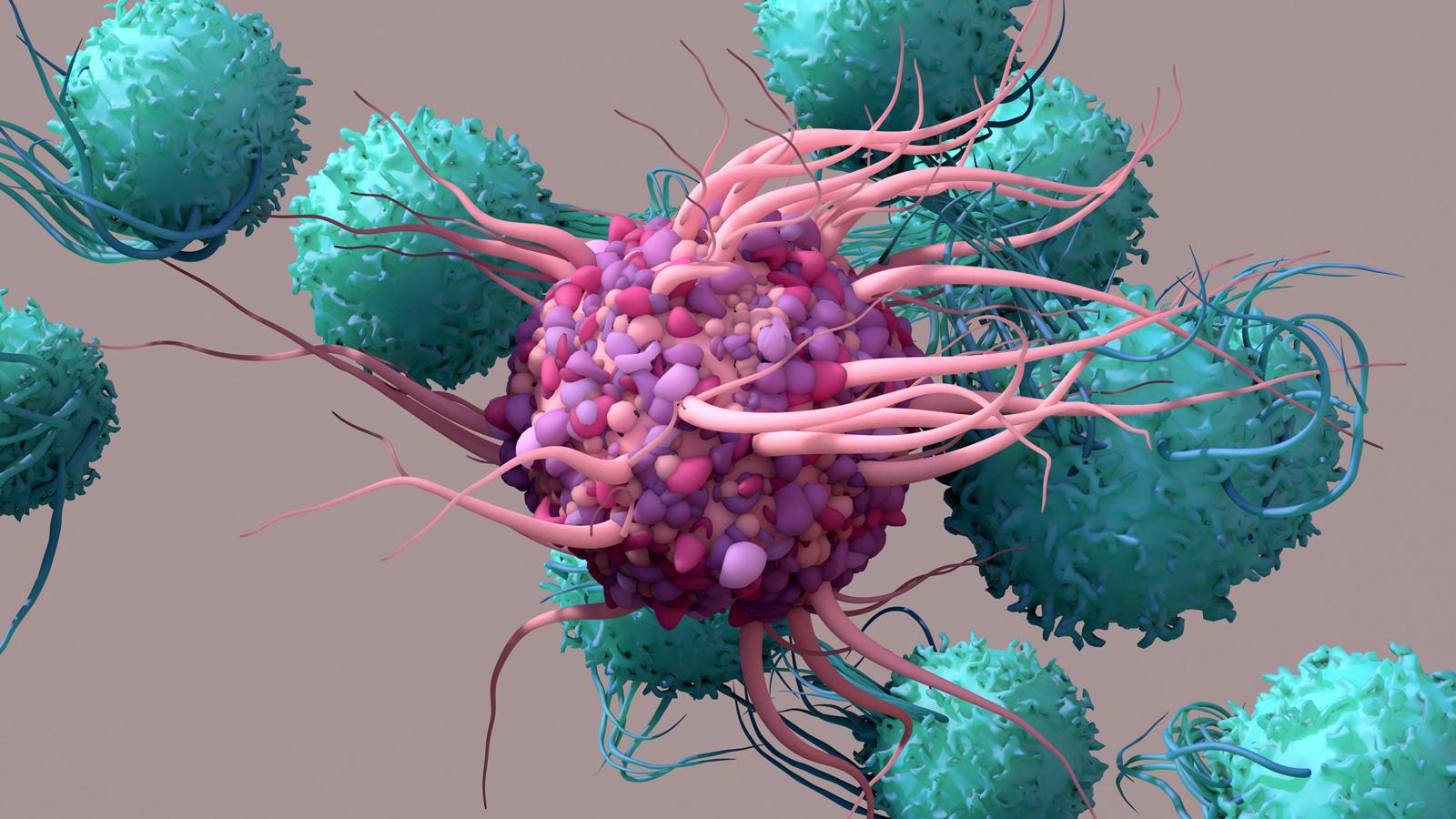
Combining new and existing immunity: A 3D approach to killing cancer
A question which has long baffled scientists, frustrated clinicians, and devastated patients is why the immune system so effectively defends against infections, but so poorly deals with cancer.
Thanks to a molecular biology-led revolution in immunotherapy, we are now beginning to strategically apply the immune defence rules that deal with micro-organisms, to attacking cancer. Importantly, no single cell type or molecule can provide effective protection against infections. It is, therefore, not surprising that targeting cancer cells with a single therapy has had limited success.
CAR-T cell therapy
Recently, a highly innovative treatment approach has emerged, involving genetically modifying a patient's own immune T-cells in the laboratory, with a gene that codes for a chimeric antigen receptor (CAR); this CAR allows that T-cell to find and bind to a cancer cell, triggering an activation cascade resulting in death of the cancer. Cancer reactive immune cells are naturally very rare; CAR technology enables a whole army of cancer fighting cells to be produced and injected back into the patient.
This CAR-mediated “seek and destroy” treatment has had stunning successes in blood cancers, with some patients actually cured. Despite this, such autologous (i.e., using the patient’s own cells) CAR-T cell therapy is limited by the number and quality of the patient’s T-cells that can be obtained because of damage through, for example, chemotherapy, radiation, exhaustive exposure to the cancer, or natural ageing. It is also prohibitively expensive.
Furthermore, with these single antigen-specific CAR-T cells, relapses are now arising from cancer cells which have escaped by mutating off the nominal target antigen. In addition, such CAR-T cells have been largely ineffective against the biologically more complex solid tumours.
Natural Killer cells
In the response to infections, it is cells of the natural “innate” immune system which are first engaged. Of these, macrophages are particularly important because they not only engulf and destroy microbes, but they can also activate other cells of the adaptive immune system to complete the elimination and also provide long-term protection. Macrophages can also detect and eradicate abnormal cells, including cancer cells, before they grow and spread.
While some macrophages are effective at killing, another form are immune suppressive and thrive in the solid tumour microenvironment (TME), promoting cancer growth. In the TME, the population of anti-tumour macrophages is relatively low. A key question is, therefore, whether the immune suppressing macrophages can be converted to those attacking cancer to improve a patient's prognosis.
Recently, Natural Killer (NK) cells have emerged as very important anti-cancer killer cells. NK cells have multiple surface receptors that recognise cancer cells, and their activation does not require complex pre-stimulation signals. In terms of killing cancer cells, they are “alert and ready to go”. The primary targets of NK cells are so-called “cell stress molecules”, which are expressed on old and damaged cells, virally infected cells, and cancer cells. Normal, healthy cells escape this killing because they lack the “stress molecules” and, in addition, they have a parallel set of receptors that directly inhibit NK cell function. When donor NK cells are transplanted into unmatched patients, there is no rejection, making them safer than T-cells, which can attack the patient’s cells.
However, as promising as NK cells are, there are three major problems thwarting their general utility: they do not divide so are numerically limited, they too are subject to the immunosuppressive TME, and they are relatively resistant to gene editing.
Blocking CD47
Cancer cells can also actively evade the immune system by multiple mechanisms. They secrete potent immune suppressing molecules. They can also express so-called “don’t eat me” receptors, such as CD47. This has a natural role in protecting healthy cells from being destroyed by macrophages; when cells become damaged or aged, the levels of CD47 are reduced and the cells can then be removed by macrophages. Cancer cells have hijacked this system, by increasing their surface expression of CD47 to promote survival by inhibiting macrophages.
Blocking CD47 on cancer cells allows macrophages to not only “eat” cancer, but also converts them from being immune suppressive to pro-cancer killing in the TME. Our strategy here is to generate dual CARs: one specific to the cancer and the other to “smother” CD47 on the cancer cell, enabling its killing by engaging the patient’s own macrophages, in addition to the cancer-specific CAR on the NK cells.
Additionally, immunosuppressive checkpoint “handbrake” genes can prevent immune cells from functioning properly. In fighting infections this is normally a good thing because it prevents immune system burn out, however, it is the last thing a cancer patient needs. By removing these genes from NK cells and macrophages, the cancer killing becomes more potent and prolonged.
3D immunity: The potential of iPSCs
The challenge is clear: can we successfully manipulate and co-engage these different immune system components to synergistically remove cancer cells, hopefully permanently - 3D immunity?
To address the limitations of autologous CAR therapy, Cartherics’ strategy involves genetic sculpturing of induced pluripotent stem cells (iPSCs), which grow indefinitely, enabling an endless supply of young, healthy immune cells to be produced. Cartherics has developed an iPSC-based technology to generate large-scale, cost-effective, clinic-ready NK (iNK) cells, and can differentiate iPSC into T-cells and macrophages. Importantly, the iPSC can be gene-edited to incorporate a CAR genetic construct and deleted of immune “handbrake” genes. Being iPSC means these functionally critical, cancer fighting genetic improvements will be transferred to all the immune killer cells they differentiate into.
Our current focus is to combine these genetic edits of the iPSC to produce “off-the-shelf” iNK cells with a CAR targeted to TAG-72, a tumour antigen present on all adenocarcinomas, such as ovarian cancer. Ovarian cancer is especially challenging, with up to 85% of patients experiencing cancer recurrence, despite undergoing surgery and chemotherapy. The 5-year survival for stage 3 and 4 patients is 41% and 31% respectively.
Several companies have embraced iPSC technologies to produce gene-edited immune cells, with the aim of advancing immunotherapies and providing more effective treatments for cancer patients. These include Shoreline, Fate Therapeutics, and Century. Numerous research groups, both in universities and independent institutions, are also at the forefront of exploring the potential of iPSCs for immunotherapy, including Stanford University, Harvard University, and the University of California. Additionally, premier medical research institutions, including the Memorial Sloan Kettering Cancer Center, are engaged in refining gene-editing and optimisation of iPSC-derived immune cells for cancer treatment.
The collective efforts of these companies and research groups contribute significantly to the advancement of iPSC technology, aiming to develop personalised and effective immunotherapies for cancer and other diseases. The future of “3D immunity” indeed looks promising.
About the authors
 Richard Boyd is chief scientific officer of Cartherics, a biotech company specialising in chimeric antigen receptor (CAR) T and CAR-NK cells. Boyd has published over 300 papers, multiple patents, and given over 400 scientific presentations. He has a long, distinguished academic career in immunology research, teaching and supervising ~100 research students, having had a long-standing career as professor at Monash University. Indeed, Boyd was a founding member of the Immunology department and was director of Monash Immunology and Stem Cell Laboratories.
Richard Boyd is chief scientific officer of Cartherics, a biotech company specialising in chimeric antigen receptor (CAR) T and CAR-NK cells. Boyd has published over 300 papers, multiple patents, and given over 400 scientific presentations. He has a long, distinguished academic career in immunology research, teaching and supervising ~100 research students, having had a long-standing career as professor at Monash University. Indeed, Boyd was a founding member of the Immunology department and was director of Monash Immunology and Stem Cell Laboratories.
 Aleta Pupovac is a cell biologist and immunologist who is passionate about translational science. She obtained her PhD from the University of Wollongong in 2015 and gained extensive research experience as a postdoctoral fellow at Swinburne University of Technology, CSIRO, and Monash University, in the fields of immunology and tissue engineering. As an early career scientist, Pupovac has contributed to the scientific community with the publication of 15 papers. Currently, she is the publications officer at Cartherics.
Aleta Pupovac is a cell biologist and immunologist who is passionate about translational science. She obtained her PhD from the University of Wollongong in 2015 and gained extensive research experience as a postdoctoral fellow at Swinburne University of Technology, CSIRO, and Monash University, in the fields of immunology and tissue engineering. As an early career scientist, Pupovac has contributed to the scientific community with the publication of 15 papers. Currently, she is the publications officer at Cartherics.












