Cold virus strain could be used as therapy for bladder cancer - study
A strain of the common cold virus can infect and kill bladder cancer cells, according to a small study, raising hopes of a potential new therapy.
Findings are based on a study from University of Surrey researchers who were investigating whether the coxsackievirus (CVA21) could be used as a novel oncolytic agent against non-muscle invasive bladder cancer (NMIBC).
NMIBC is found in the tissue of the inner surface of the bladder and is the tenth most common cancer in the UK with approximately 10,000 people each year diagnosed with the illness.
This was only a phase 1 study involving 15 patients, but study authors said that findings are strong enough to suggest the virus could be a potential new therapy.
Authors pointed out that current treatments for this cancer are problematic – a common option is an invasive procedure called transurethral resection that removes all visible lesions but has a high recurrence rate from 50%-70%.
The op also has a high tumour progression rate between 10%-20% over a period of two to five years.
Another common course of treatment, immunotherapy with the live bacterium Bacille Calmette-Guerin, has been found to have serious side effects in one third of NMIBC patients while one third do not respond to the treatment at all.
The CANON study was based around a novel coxsackievirus modified to target intercellular adhesion molecule 1 (ICAM-1), known as CAVATAK.
This was given to patients via a catheter to the bladder a week before pre-scheduled surgery to remove tumours.
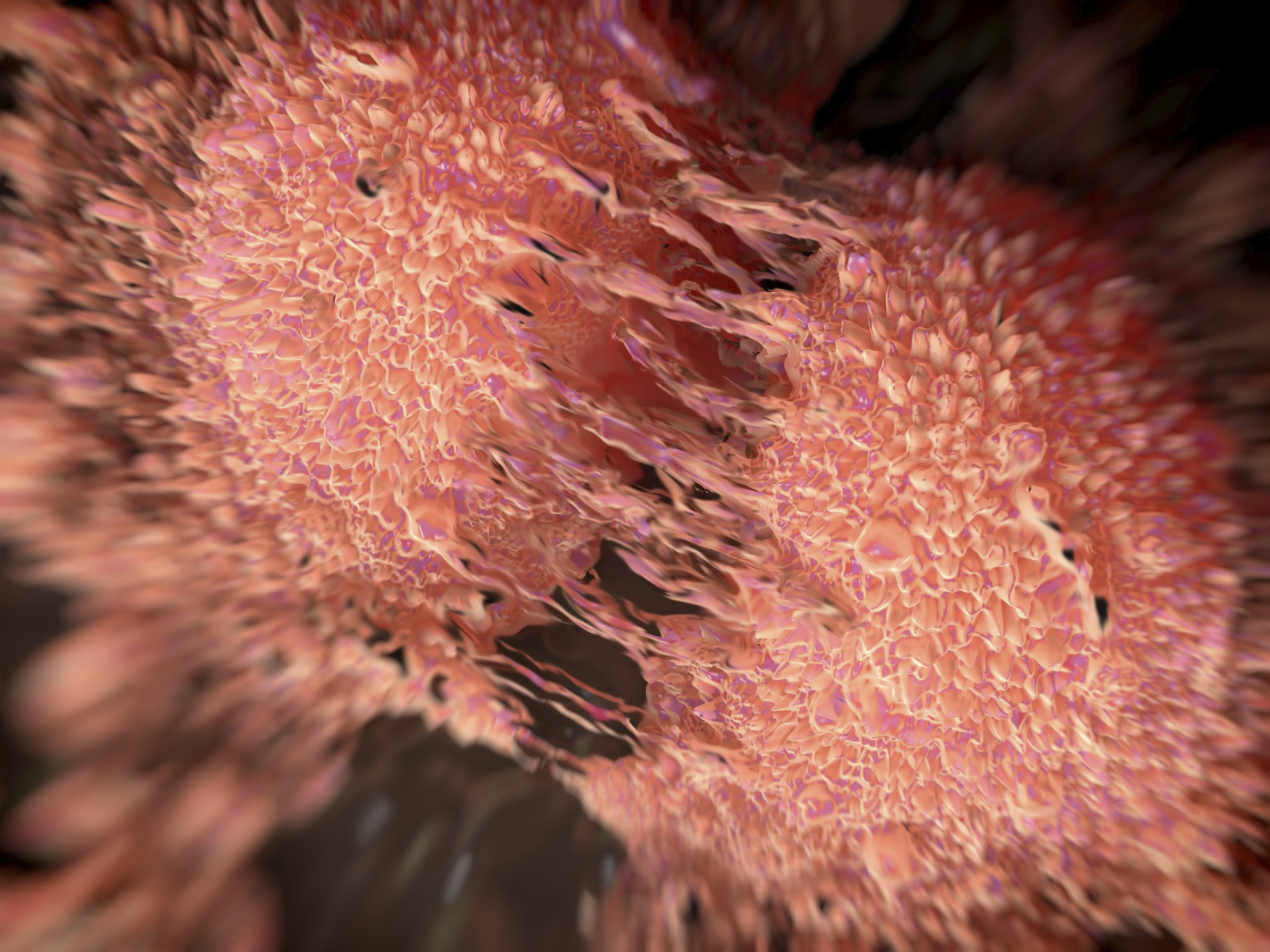
Examination of tissue samples post-surgery discovered that the virus was highly selective, targeting only cancerous cells in the organ and leaving all other cells intact.
The virus was found to have infected cancerous cells and replicated itself causing the cells to rupture and die.
Urine samples taken from patients on alternate days detected ‘shedding’ from the virus indicating that once virally infected cancer cells had died, the newly replicated virus continued to attack more cancerous cells in the organ.
All signs of the disease disappeared in one patient, and the evidence of cancer cell death was present in all other patients.
They concluded that the virus had turned the tumours from “cold” ones ignored by the immune system, to “hot” ones that are visible to and attacked by the body’s defences.
Authors concluded that an “acceptable” safety profile of CAVATAK, proof of viral targeting, replication and tumour cell death, and the creation of “immunological heat” around tumours indicate that CAVATAK “may be potentially considered as a novel therapeutic for NMIBC.”
Hardev Pandha, principal investigator of the study and professor of oncology at the University of Surrey, said: “Coxsackievirus could help revolutionise treatment for this type of cancer. Reduction of tumour burden and increased cancer cell death was observed in all patients and removed all trace of the disease in one patient following just one week of treatment, showing its potential effectiveness. Notably, no significant side effects were observed in any patient.”












