Case Study: MGI and Alacris Theranostics
As World Cancer Day approached this year, the increasing focus on precision oncology continued apace.
Here, Professor Marie-Laure Yaspo, Chief Scientific Officer at Alacris Theranostics, discusses her work on molecular tumour profiling, and how MGI’s technology has assisted in acceleration of that research.
Understanding the tumour landscape and biology
Prof Yaspo was involved in the Human Genome and International Cancer Genome projects. During that time, it became obvious that, with a deep analysis of genomes and transcriptomes, a vast amount of information could be gathered on both tumour landscape and biology for understanding how to personalise therapy.
It was, in fact, the idea of translating this research for the development of innovative cancer diagnostics that led to the foundation of Alacris Theranostics, pursuing the idea of predicting drug response in the future, based on the deep molecular profile of the tumour for each patient. Because every patient is different; and every tumour is different.
And so, Alacris evolved from research and development projects into a biotech company focusing on precision oncology and comprehensive tumour profiling. Co-founded by Dr Yaspo, together with Hans Lehrach and George Church, Alacris’ vision is to develop solutions enabling implementation of translational oncology approaches for clinical use by any hospital or oncology unit offering comprehensive molecular diagnostics to cancer patients.
Multi-omics for tumour profiling
 A prominent trend in analytical fields recently has been multiomics in life sciences, or multimodal analysis, where a more comprehensive picture of multiple studies and different techniques can present different aspects of a system. In tumour profiling, DNA, transcriptome, and proteins are profiled – “the more information, the better,” according to Yaspo, “the deeper the data, the easier it is to find your targets.”
A prominent trend in analytical fields recently has been multiomics in life sciences, or multimodal analysis, where a more comprehensive picture of multiple studies and different techniques can present different aspects of a system. In tumour profiling, DNA, transcriptome, and proteins are profiled – “the more information, the better,” according to Yaspo, “the deeper the data, the easier it is to find your targets.”
It’s just a matter of having the right analysis system and the right strategy to look at the data.
Within tumour types, there are communalities, but also differences. There are other cells that co-infiltrate the tumour mass, such as immune cells like regulatory T-cells, which play a major role in the tumour growth, and drug response.
“During the tumour analysis, when we sieve the most relevant variants, we also […] flag the most important changes, […] not only the mutations, but also the most drastic changes of gene expression,” explained Yaspo. “We can chart the microenvironment profile.
“We are using algorithms that can predict if a variant is potentially damaging, pathogenic, or not,” Yaspo continued. “Then, we match the changes to drug databases to assess whether there is a potential matched treatment for those particular, actionable alterations.”
The benefits of comprehensive profiling for guiding combination therapy
Today, cancer treatment no longer relies on only one alteration, or on one single drug.
“Most of the time, it’s a combination therapy strategy” said Yaspo. “And for combination therapy, you need to really see through the tumour landscape [to know how] to tailor the best possible treatment. In the analysis programs that we use, we have many steps, using several algorithms that are aggregated together. But to find the needle in the haystack, you need to have the haystack to look at first, and that's what we deliver: deep data for better analysis.”
“In the tumour report, we list patient-match-therapy choices, but then it remains the oncologist's choice to decide one drug or a combi, or none at all, depending on many clinical factors and the patient status,” said Yaspo. “Our job is to read out the tumour story, informing the clinician on actionable alterations […] It's still the choice of the oncologist to decide what to do next and what treatment to propose.”
“There are about 25 drug categories that directly hit a mutated product, that is to act on the structurally changed protein, but other targeted drugs are more mechanistic, such as those targeting homologous recombination deficiency pathways or the family of MEK inhibitors for instance,” Yaspo described. "There is this paradigm shift in treatment strategies towards tumour-agnostic and mechanistic approaches […] That's where the comprehensive profiling is really supporting that paradigm change.”
The trend in molecular diagnostics goes towards multimodal solutions
 “The large majority of clinical units who use multimodal tests, and that is still a restricted number of units, most often use targeted panels,” Yaspo said. “So, they have only a few targets in the RNAs that can they look at, but unfortunately the bulk transcriptome information is not yet widely used at all. And again, in the bulk information, you profile not only the tumour cells, but also the cells which accompany the tumour and actually participate in the growth of the tumour. The immune environment is incredibly important to the tumour. And this is why there are so many immuno-drugs and immune checkpoint inhibitors in development, which efficiency needs to be evaluated by following up the molecular response of the tumour to treatment. The trend is now evolving. We do see this paradigm change prompting the need for multimodal comprehensive diagnostics.”
“The large majority of clinical units who use multimodal tests, and that is still a restricted number of units, most often use targeted panels,” Yaspo said. “So, they have only a few targets in the RNAs that can they look at, but unfortunately the bulk transcriptome information is not yet widely used at all. And again, in the bulk information, you profile not only the tumour cells, but also the cells which accompany the tumour and actually participate in the growth of the tumour. The immune environment is incredibly important to the tumour. And this is why there are so many immuno-drugs and immune checkpoint inhibitors in development, which efficiency needs to be evaluated by following up the molecular response of the tumour to treatment. The trend is now evolving. We do see this paradigm change prompting the need for multimodal comprehensive diagnostics.”
Case studies: Refractory melanoma and paediatric B-cell leukaemias
Alacris ran a molecular study on refractory melanoma, financed by the German government, together with the Max Planck Institute for molecular Genetics and the Charité Compréhensive Cancer Center in Berlin.
“The project focus was to implement comprehensive multi-modal diagnostics in the clinics, which ran over more than five years [and] we had a cohort of 100 in at the end of the project,” explained Yaspo. “We published the data, we could see a benefit for about 30% of the patients, which is very significant."
“When we started this analysis [...] we really had to read all the gene fusions from the RNA-seq, and we did and could define targetable alterations to about 30% of the patients,” noted Yaspo. “And that has been a very important teaching experiment in the learning curve for us and for the tumour board to see how far the clinical use can be extracted from this data.”
Another focus area of the company’s research is in diagnostics for paediatric acute lymphoblastic leukaemias, also at the Charité, with Dr Cornelia Eckert.
“[There] as well, we make [extensive] use of bulk RNA-seq,” said Yaspo. “We will add whole genome sequencing soon, but the RNA-seq has been what they have needed. We have been doing that for the past three years now, and here, again, harnessing bulk RNA-seq supported the design of clinical trials.”
Reduced read duplication rates with MGI’s technology
The evolving landscape of drug development has, of course, a part to play, interacting with technological advances in sequencing.
“There is a huge development of new drugs and immune-drugs, which are important as a therapy response marker,” noted Yaspo. “Economically now, with the cost of sequencing [having] gone down significantly, the costs of non-targeted comprehensive diagnostics is very competitive and aligned to that of the so-called large panels.”
“A great advantage is the format of the sequencer,” continued Yaspo. “You could have a very small sequencer, but for our strategy we sequenced about 40 to 50 Gb per tumour. You get better data, the format is more flexible, and the low cost allows you to really introduce that strategy in the routine at [an] affordable price. So, we are within a range that is compatible with the health insurance reimbursement system and to [a] turn-around time [that] also fits the patient journey. We could do the procedure within one week from tumour samples to giving the report nowadays, and that's really very fitting."
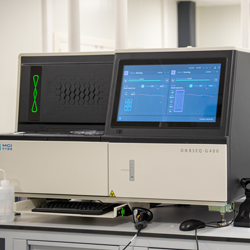
 MGI’s DNBSEQ-G400 is the main instrument used by Alacris, but this year the DNBSEQ-T7 was implemented, also. DNBSEQ-G400 is built with a new Flow Cell system that supports a variety of different sequencing modes. DNBSEQ-T7, meanwhile, can output seven terabytes of high-quality data within 24 hours and is applicable to whole genome sequencing, deep exome sequencing, epigenome sequencing, transcriptome sequencing, tumour panel, and other data-intensive projects.
MGI’s DNBSEQ-G400 is the main instrument used by Alacris, but this year the DNBSEQ-T7 was implemented, also. DNBSEQ-G400 is built with a new Flow Cell system that supports a variety of different sequencing modes. DNBSEQ-T7, meanwhile, can output seven terabytes of high-quality data within 24 hours and is applicable to whole genome sequencing, deep exome sequencing, epigenome sequencing, transcriptome sequencing, tumour panel, and other data-intensive projects.
Whole genome sequencing and identifying chromosome breakpoints
But what's special about the cases where the clinicians want to do whole genome sequencing?
“That’s an important question,” admitted Yaspo. “The whole genome sequencing provides a base resolution of the genome rearrangements, which you cannot reach with the exome, because the exome would interrogate only the exons, representing only a small part - about 5% of the whole genome. Typically, haematological cancers display gene fusions, gene rearrangements, which bring two different parts of the genome originally far from each other into proximity, creating a fusion product.”
“The fusion products are detected in the RNA sequence most of the time, however, this does not give us the precise genomic breakpoint,” she said. “Because when you break a chromosome, most often the breakpoint occurs within a non-coding region. Knowing the exact breakpoint […] is essential for designing tests to detect the MRD (minimal residual disease) to follow-up and monitor potential relapse of the disease. And to detect these very low-frequency events you need to know the breakpoint.”
About MGI

MGI Tech Co. Ltd. (or its subsidiaries, together referred to as MGI), headquartered in Shenzhen, is committed to building core tools and technology to lead life sciences through intelligent innovation. Based on its proprietary technology, MGI focuses on research & development, production and sales of sequencing instruments, reagents, and related products to support life sciences research, agriculture, precision medicine, and healthcare. MGI is a leading producer of clinical high-throughput gene sequencers**, and its multi-omics platforms include genetic sequencing**, medical imaging, and laboratory automation. MGI's mission is to develop and promote advanced life science tools for future healthcare. For more information, please visit the MGI website or connect with us on X, LinkedIn or YouTube.











