UK medical journals spar over breast cancer screening study
Screening women for breast cancer in their 40s rather than their 50s could save lives, say the authors of a new Lancet Oncology study, although that finding has been challenged by other experts.
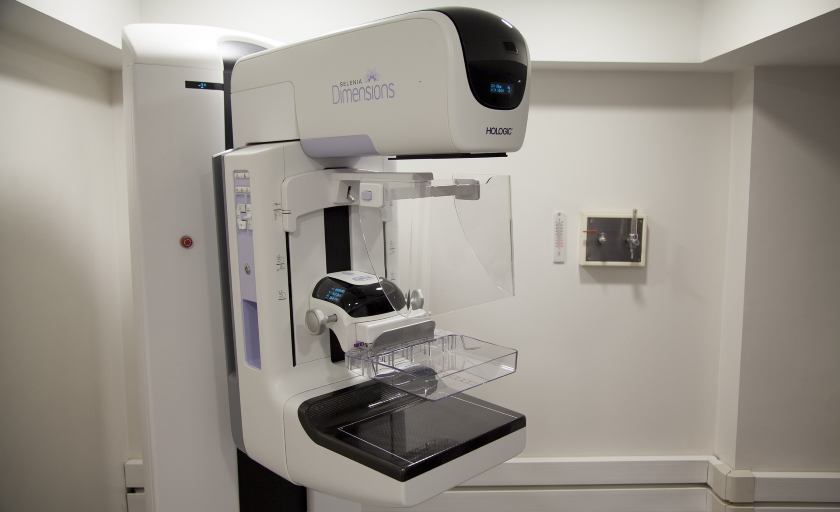
Lowering the age that women start to routinely get mammograms was associated with a relative reduction in breast cancer mortality without leading to ‘over-diagnosis’ – in other words detecting minor changes that may not turn into full-blown cancers – according to the scientists.
The UK currently offers mammograms every three years to women aged 50 to 70, but in this trial – led by Prof Stephen Duffy of Queen Mary University in London – 160,000 women aged 40 or 41 were randomised to either once-yearly mammograms or no screening.
The best timing for screening is a hotly-debated topic, and the British Medical Journal ran an article challenging the Lancet Oncology findings on the day of publication, citing experts who dismissed the findings as “misleading rhetoric.”
Cancer Research UK also chimed in, saying that even with the new study it is still unclear if reducing the breast screening age “would give any additional benefit compared to the UK's existing screening programme.”
It found an initial reduction in breast cancer deaths from screening, but this disappeared over time, according to the charity, which believes more effort should be devoted to restoring access to current screening and other cancer-related NHS services that have been disrupted by the coronavirus pandemic.
The Lancet Oncology paper found that after almost 23 years of follow up, there were 83 breast cancer deaths among the almost 54,000 randomised to the screening group, versus 219 among more than 100,000 in the no-screening control group.
The results are similar to those revealed 15 years into the follow-up period, but over the longer term there was little difference in mortality between the groups. Overall, the number of deaths per 10,000 women was 16 in the screening group and 21 for the controls.
The benefit was seen mostly in the first 10 years, but the reduction in breast cancer mortality was maintained in the long term at about one life saved per 1,000 women screened, according to the researchers.
Vinay Prasad, associate professor at the University of California, San Francisco, told the BMJ: “’Saves lives’ means that women, as a result of doing this, live longer than those who do not do it.”
He went on to say that “did not occur in this dataset” adding that in fact it was “quite the opposite,” given that all-cause mortality data found no difference between the groups.
The study recruited women from the late 1990s, when mammography may not have been as effective as today. On the other hand, the cost of extending the screening programme could be significant and could be hard to justify given the small reductions in breast cancer deaths recorded.
“Compared to the existing screening programme, in the younger age group, six times more women would need to be screened to save one life,” said CRUK.
“Many women received false positive results and some women would have been over-diagnosed with cancers that would never have gone on to cause them harm,” it added.
Image by Elías Alarcón from Pixabay













