NHS England confirms HIV prevention funding - but only via clinical trial
NHS England has confirmed that it will fund HIV prevention programme based around pre-exposure prophlyaxis (PrEP) with Gilead’s Truvada.
The announcement follows months of legal wrangling after NHS England axed plans for a national PrEP programme, but was last month forced to reconsider after a court challenge from campaigners.
However there remain doubts about just how extensive NHS England's commitment is, as it says the money will be spent on a "large scale clinical trial" - suggesting that long-term funding is not guaranteed, and contingent on results.
The HIV initiative was part of a raft of specialised treatments commissioned by NHS England as part of an annual prioritisation process.
Following last month’s Court of Appeal ruling that NHS England has the power, but not the obligation to fund PrEP, commissioners have opted to launch the clinical trial early in the 2017/18 financial year.
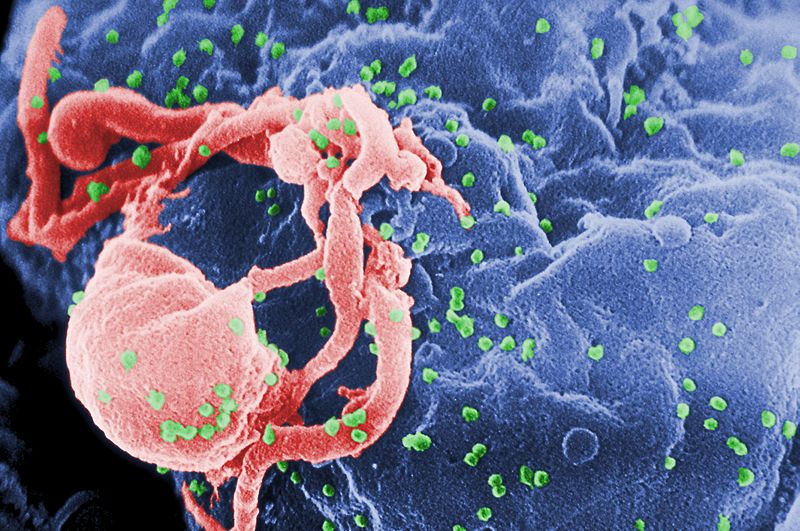
Truvada (emtricitabine+tenofovir) has been shown to have a protective effect, and can in some cases stop HIV becoming established in the body.
NHS England said that although the clinical effectiveness of PrEP is strong, advice from Public Health England has highlighted “outstanding implementation questions” that should be answered before rolling out PrEP across England.
Around 10,000 people are expected to take part in the trials over three years, fully funded by NHS England, which will work in partnership with local authorities, councils and Public Health England to implement the findings.
The trial will cost around £10 million and NHS England will now approach Gilead, as well as generic manufacturers, to participate.
Although NHS England has not provided further details, the clinical trial will likely address issues such as how to get the drug to those who most need it, and the ramifications of this for the NHS, and the clinics run by local authorities that will prescribe the drug.
Dr Jonathan Fielden, director of specialised commissioning and deputy national medical director, NHS England said: “We’re pleased to be able to announce funding not only for ten new specialised treatments but also a new ground breaking national programme for PrEP that will benefit at least 10,000 people.
“This has, in part, been made possible by the willingness of many pharmaceutical and device companies to come forward with lower and more responsible prices. Continuing this constructive joint working will enable us to fund more new drugs and treatments in the future.”
Kat Smithson, policy and campaigns manager at the National AIDS Trust, which was behind the legal campaign to get PrEP funded, cautiously welcomed the announcement.
But she said the “devil was in the detail” of the clinical trial. “We have to make sure that the way it is implemented does work.”
“The NHS’s intention is to treat as many people as possible and we broadly welcome this,” said Smithson, who noted that PrEP will not just be restricted to certain groups.
Public Health England has said that there are around 13,500 people living in the UK with an undiagnosed infection and around 101,200 people living with HIV in the country
Smithson said: “This shows us we do need some changes in the prevention strategy.”












