Healthcare AI from Cera ‘could save NHS and UK £1bn a year’
An artificial intelligence-powered home healthcare model that aims to keep elderly people out of hospital and residential care and in their own homes would save £1 billion ($1.26 billion) a year by 2026 if it is rolled out nationwide.
That’s according to a study by London-based AI consultancy Faculty, which looked at data from the use of Cera’s Digital Care Plan (DCP) platform in around 150 of the UK’s 382 local authorities, as well as 29 of 42 NHS Integrated Care Boards.
The analysis concluded that the use of DCP reduced hospitalisations in the over-65s by 52% to 70% – preventing 233 emergency admissions – by predicting falls, tracking symptoms, and mobilising frontline nurses and carers to respond to high-risk alerts and treat common conditions like urinary tract infections at home.
It is already saving the NHS £1 million a day from reduced A&E waiting times and lower hospital and care home admissions, according to the report, which estimates that could increase to £2 million per day in 2025 and more than £3 million in 2026 if additional authorities and ICBs adopt the system.
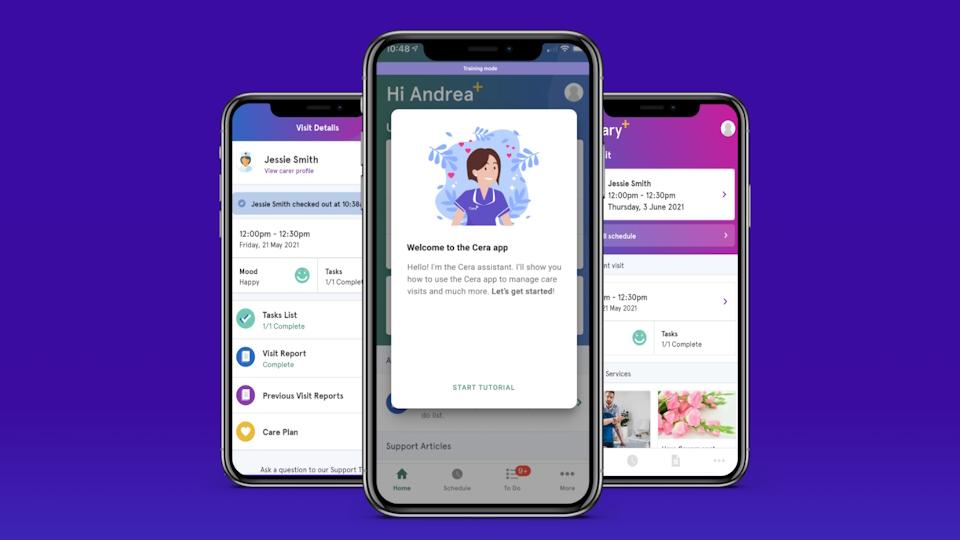
The app-based platform records a range of information, including care support, risk assessments, medication administration and adherence, and contact with healthcare staff.
According to Faculty, which created the report on the technology for the NHS, it is freeing up more than 1,210 hospital bed days each month, each of which costs the NHS around £460.
The data comes shortly after figures from the Office for National Statistics (ONS) found that one in five people in England are waiting for hospital care – a might higher figure than NHS estimates – with 9.7 million waiting for treatment, an appointment or a test. NHS estimates don’t include so-called ‘hidden waits’ – in other words, patients who have started treatment and are waiting for follow-up care.
In 2023, Royal College of Emergency Medicine data suggested that long waiting times were linked to more than 250 deaths a week.
Cera – founded by former frontline NHS doctor Ben Maruthappu eight years ago – says that 2023 data shows that the over-65s accounted for two-thirds of the 150,000 patients forced to wait 24 hours in A&E before being admitted to hospital, in 2023 a delay that could also lead to needless patient deaths.
“As our population ages and pressure on in-patient services increases, taking care out of hospitals and residential settings and into patients’ homes is fundamental to the future of our health and social care system,” said Hugh Neylan, head of health at Faculty.
“It’s exciting to see cost savings already being delivered by AI, and this will only grow as their adoption increases.”













