First CRISPR drug Casgevy gets swift second approval
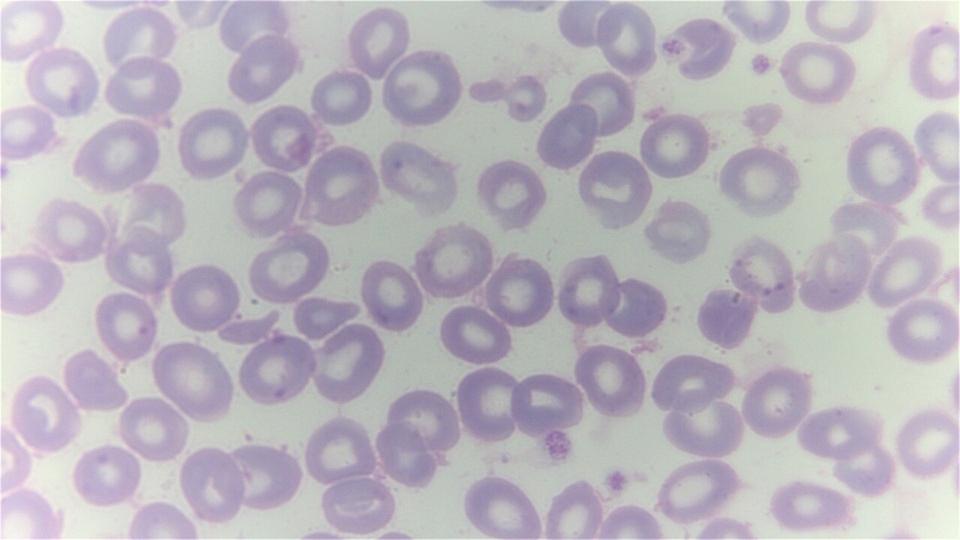
The FDA has lost no time in approving Vertex Pharma and CRISPR Therapeutics pioneering gene-editing therapy Casgevy for its second use, approving the drug for transfusion-dependent beta thalassaemia (TDT) more than two months ahead of deadline.
Casgevy (exagamglogene autotemcel or exa-cel) became the first drug based on the CRISPR/Cas9 gene-editing technology to be approved towards the end of last year, when it was cleared by the FDA for sickle cell disease (SCD). The UK was the first country to give the go-ahead for the drug last November, backing it for both TDT and SCD.
“On the heels of the historic FDA approval of Casgevy for sickle cell disease, it is exciting to now secure approval for TDT well ahead of the PDUFA date,” said Reshma Kewalramani, Vertex’s chief executive.
“TDT patients deserve new, potentially curative treatment options, and we look forward to bringing Casgevy to eligible patients who are waiting,” he added.
Casgevy was the first drug to be licensed based on CRISPR, which earned its discoverers a Nobel Prize in 2020. The one-shot therapy is an ex vivo application of the technology, meaning that bone marrow stem cells are taken from patients and gene-edited outside the body before reinfusing them to treat disease.
CRISPR-based therapies are also being developed for in vivo use, in which the gene editing occurs within the body, but these are still at the experimental stage.
Vertex said there are around 1,000 TDT patients in the US eligible for treatment with Casgevy, which can be used in individuals aged 12 years or over with the disease. Patients with TDT require frequent blood transfusions and iron chelation therapy throughout their lives and generally don’t survive beyond their late 30s.
In trials, Casgevy was shown to improve the proportion of patients who were transfusion-independent for at least 12 consecutive months.
As it requires a stem cell transplant, the therapy is only available to patients who are fit and healthy. Vertex and CRISPR say they plan to provide it through a network of independently operated, authorised treatment centres and have set a list price of $2.2 million for both TDT and SCD.
It is an alternative to bluebird bio’s Zynteglo (betibeglogene autotemcel), a cell-based gene therapy that was approved by the FDA to treat TDT in 2022 and launched at a one-off cost of $2.8 million.
A recent study estimated the lifetime cost of TDT to be $5.4 million, spit between $1.6 million for the transfusions themselves and $3.7 million for chelation therapy to remove excess iron from the body.
Zynteglo has been slow to gather momentum since its launch, but analysts at Evaluate are predicting take-up of Casgevy could be faster, with sales reaching $2.6 billion by 2028.
bluebird could fare better with its new cell-based gene therapy for SCD, Lyfgenia (lovotibeglogene autotemcel), which was cleared by the FDA in December and has a list price of $3.1 million.
Both Casgevy and Lyfgenia are highlighted in a recent Clarivate report among 13 potential “blockbuster and gamechanger” drugs to watch in 2024.
Image by Dr Graham Beards via Wikimedia












