Biomarker study raises hope of better depression therapies

Researchers may have identified imaging-based biomarkers that could be used to identify different subtypes of major depressive disorder (MDD) and potentially lead to the development of better treatments.
The many millions of people worldwide with depression are usually lumped into a single category, despite having considerable diversity in terms of emotional and cognitive symptoms, which could explain why current therapies for MDD lack efficacy for up to one-third of patients.
There have been attempts to identify different forms of MDD using clinical symptoms, such as melancholic depression, atypical depression, and seasonal affective disorder and, while these pointed to some differences in neurophysiology, they have not led to targeted forms of treatment.
A team of scientists led by Dr Mingrui Xia of Beijing Normal University in China used resting-state functional MRI scans collected from more than 1,000 MDD patients and over 1,000 matched control subjects to look for differences in connectivity among different regions of the brain.
The study relied on the ‘normative’ model of analysis, which uses data from a large reference population to identify and quantify individual deviations. The approach works “much like the growth charts used by paediatricians,” according to the scientists, who have published their work in the journal Biological Psychiatry.
‘Connectome’ is key
They found two neurobiologically distinct subtypes of MDD, with different abnormality patterns and clinical characteristics, raising the possibility for personalised diagnosis and treatment of depression for the first time.
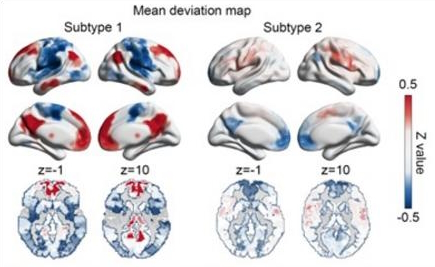
One subtype of patients showed increased brain connectivity in the default mode network, limbic, and subcortical areas, and reduced activity in the sensorimotor and attention areas. In the second subtype, that pattern was reversed and the change in connectivity was less pronounced.
One consequence of the changes could be a difference in the tendency to ruminate or fixate on past, generally negative experiences - the repetitive thoughts seen in some people with MDD that can take a toll on attention and the ability to manage difficult situations.
Along with different imaging patterns, the two groups also had distinctive scores on depression symptom sales and tended to respond differently to treatment, according to Xia.
“The implications of this research are far-reaching, providing valuable insights into the development of imaging-based candidate biomarkers,” he said.
“These biomarkers have the potential to guide future precise diagnostic and treatment strategies tailored to each patient’s specific neurophysiological subtype. By embracing the concept of neurophysiological subtypes, we can potentially revolutionise the field of mental health by enabling clinicians to personalise treatments based on an individual’s unique connectome characteristics.”
Photo by Milada Vigerova on Unsplash.












