Better tasting antibiotics could reduce resistance
Older antibiotics, reformulated to make them more palatable to patients, could be part of the answer to the antibiotics crisis, a generics trade body has said.
Medicines for Europe is launching a 'Value Added Medicines' group that will champion new uses of older drugs, or when these drugs are changed to bring new value to patients.
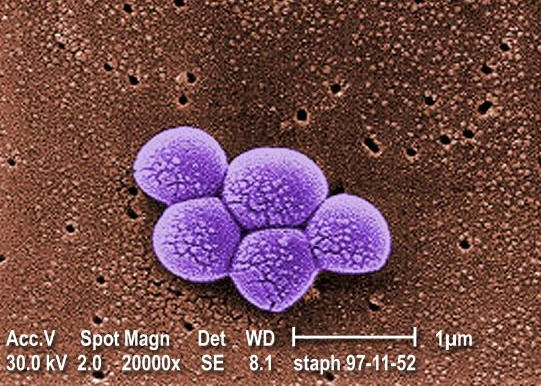
One such example is in the field of antibiotics, where failure to finish a course can lead to resistant strains of bacteria developing in patients.
So finding ways to make these drugs more palatable, either through a different formulation that tastes better, or perhaps a different method of administration, could reduce the likelihood of resistant strains emerging.
Professor Mondher Toumi, professor at the University of Aix-Marseille, and CEO of life sciences consulting firm, Creativ Ceutical, told an online press briefing: “Fixed dose combinations or reformulations that will improve compliance could minimise the risk of resistance related to patient behaviour.”
In a white paper outlining the many uses of so-called value-added medicines, Toumi noted that the European Centre for Disease Prevention and Control and the World Health Organisation are worried that poor adherence to antibiotics could lead to resistant strains.
Meanwhile, the row continues over a recommendation last month by economist Lord O’Neill that pharma companies should pay a levy or develop new antibiotics.
O’Neill’s “pay or play” proposal has been heavily criticised by the Ethical Medicines Industry Group (EMIG), representing small and medium-sized pharma.
EMIG chairman Leslie Galloway said: “It is the most outrageous thing I have ever heard. Companies that have no history in being involved with antibiotics, delivering highly effective medicines, are being fined for not researching antibiotics.
“This is not a drug problem it is a whole global problem. We will probably have to stockpile [new antibiotics] like vaccines, to make sure resistance does not occur. People respond to incentives, not threats.”
He said the cause of the problem in the UK is funding, as only 8.5% of GDP is spent on health while France and Germany spend around 11%.
Big pharma, represented by the Association of the British Pharmaceutical Industry (ABPI), as well as European and global federations, said that the “pay or play” proposal would undermine goodwill from pharma companies committed to finding new antibiotics.
Photo courtesy Public Health Image Library












