ASH: Regeneron plays its PNH hand
Regeneron will have a tough job taking on AstraZeneca’s big-selling Ultomiris in the market for paroxysmal nocturnal haemoglobinuria (PNH) therapies – but new biomarker data suggests it could have a shot.
Updated results from the ACCESS-1 trial comparing combination therapy with pozelimab and cemdisiran (poze-cemdi) to Ultomiris (ravulizumab) indicate that Regeneron’s duo may be able to achieve and maintain greater disease control, as measured by lactate dehydrogenase (LDH) levels.
The data – shared at the American Society of Haematology annual congress – showed that, in PNH patients previously untreated with complement inhibitors, 96% of those treated with poze-cemdi achieved adequate LDH control, compared to 80% of the arm treated with AZ’s drug, over 26 weeks of follow-up. Normalisation of LDH levels was seen in 93% and 65% of patients, respectively.
Ultomiris is a complement C5 inhibitor that has become a mainstay of PNH treatment, helping it become a $2.8 billion product in the first nine months of 2024. It offers reduced dosing frequency compared to its predecessor Soliris (eculizumab), which added just over $2 billion to AZ’s revenues in the same period.
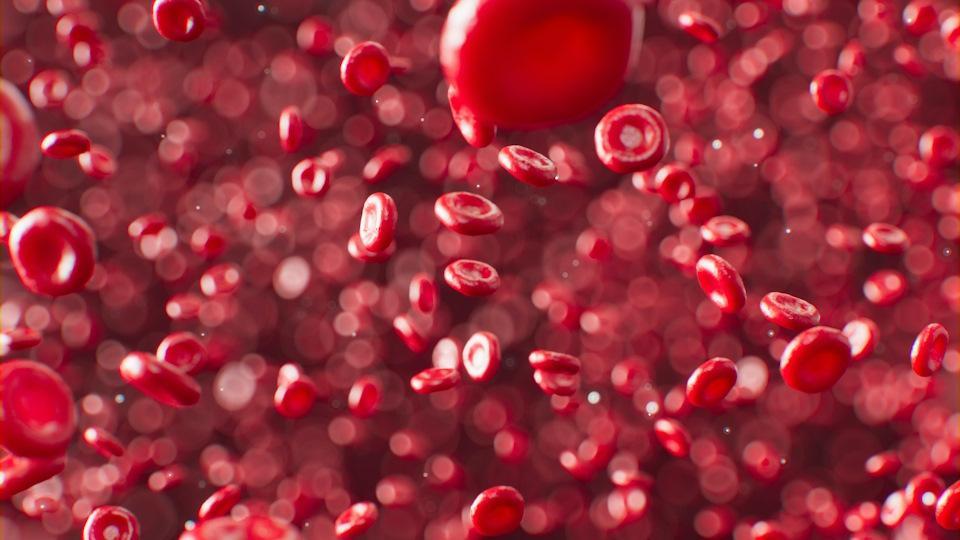
Like AZ’s drugs, pozelimab is a C5 inhibitor, but is co-administered with cemdisiran, an investigational siRNA therapeutic developed with Alnylam under a $1 billion alliance agreed in 2019 that reduces circulating levels of C5 in the blood. Regeneron says this makes the combination a first-in-class prospect for PNH – a rare disease that destroys red blood cells. LDH is released when the red blood cells break down, so serves as a surrogate marker for anti-PNH therapies.
Poze-cemdi also has the distinction of being administered subcutaneously, while Ultomiris needs to be given using an intravenous infusion.
“C5 inhibitors are widely considered the mainstay of PNH treatment, but a proportion of patients still do not achieve adequate control of intravascular haemolysis, may experience residual anaemia, and may feel significant treatment burden, as many of these therapies require clinic or home visits for intravenous delivery,” said ACCESS-1 trial investigator Christopher Patriquin, of the University of Toronto.
He added that the combination achieved “complete, rapid, uninterrupted, and durable inhibition” of C5 and noted that, if additional data reinforces these findings, poze-cemdi could “help transform what may be possible for many people with PNH.”
Regeneron and Alnylam are now waiting for the results of a second cohort in ACCESS-1 comparing poze-cemdi with Soliris, and are also running trials of the combination in other complement-mediated diseases, including generalised myasthenia gravis (gMG) and geographic atrophy (GA) secondary to age-related macular degeneration (AMD).
Pozelimab has already been approved for marketing by the US FDA under the Veopoz trade name for the treatment of adult and paediatric patients aged one year and older with CD55-deficient protein-losing enteropathy (PLE), also known as CHAPLE disease, which is an ultra-rare disorder leading to life-threatening blood clots. Soliris is currently used off-label to treat CHAPLE.












