Spotlight on...osteoporosis

Siobhan Hallmark
National Osteoporosis Society
This month’s article in our ‘Spotlight on...’ series highlights the bone disease, osteoporosis, following the global osteoporosis awareness day on the 20th October. Siobhan Hallmark discusses the symptoms, risks and treatments available for patients with osteoporosis and shares her thoughts on what needs to be done for these patients in the future.
What is osteoporosis?
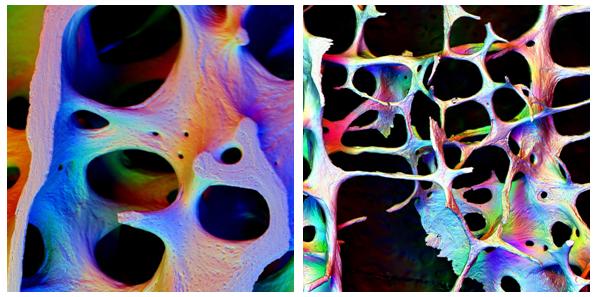
Osteoporosis occurs when the struts that make up the mesh like structure within bones become thin, causing them to become fragile and break easily, often following a minor bump or fall. These debilitating fractures are known as ‘fragility fractures’.
Figure 1: An example of a healthy bone, compared to an osteoporotic bone. Credit: Alan Boyde.
Osteoporosis is very common – three million people in the UK are estimated to have osteoporosis and there are about 300,000 fragility fractures in the UK every year. Shockingly, one in two women and one in five men over the age of 50 will break a bone, mainly because of poor bone health.
What are the symptoms to look out for?
Osteoporosis is often termed the ‘silent disease’ as there are no symptoms prior to a fracture and for many people the first sign of osteoporosis is a wrist fracture. Once a person has broken a bone, their risk of breaking another bone increases dramatically.
Wrist fractures can occur after minor falls and ribs can break as a result of something as simple as coughing or sneezing. Fractures that compress the vertebrae can cause extreme pain and can lead to loss of height and major changes to body shape that constrict the internal organs, which can set off all sorts of digestive and respiratory problems
 ,
"Osteoporosis is often termed the ‘silent disease’ as there are no symptoms prior to a fracture..."
 ,
Hip fractures are all too common and can be severely debilitating, causing loss of mobility and increasing the chance of an early death.
BUT osteoporosis and fragility fractures are not an inevitable part of ageing and much can be done to prevent them.
Who is at risk?
The factors that can put people at risk of osteoporosis and fractures include:
• Genes – Our bone health is largely dependent on the genes we inherit from our parents. In fact, if one of your parents has broken a hip, you may be more susceptible to developing osteoporosis and fragile bones.
• Age – Bone loss increases in later life so by the age of 75 about half of the population will have osteoporosis. As we get older bones become more fragile and more likely to break.
• Gender – Women have smaller bones than men and they also experience the menopause, which accelerates the process of bone turnover. The female hormone oestrogen has a protective effect on bones. At the menopause (normally around the age of 50) the ovaries almost stop producing this hormone reducing the protection it gives to bones.
• Race – People who are Black Afro Caribbean are at a lower risk because they have bigger and stronger bones.
• Low body weight – If you have low BMI (body mass index) below 19g / m2 you are at greater risk of developing osteoporosis.
• Previous fractures – If you have already broken bones easily, including in the spine, then you are much more likely to have fractures in the future.
There are also some medical conditions that can increase your risk of osteoporosis:
• Rheumatoid arthritis.
• Low levels of the sex hormone oestrogen in women as a result of early menopause, having a hysterectomy with removal of ovaries (before the age of 45), anorexia nervosa or Turners syndrome. Excessive exercise can also reduce hormone levels.
• Low levels of the sex hormone, testosterone, in men following surgery for some cancers. Some rare conditions that men are born with such as Klinefelters disease or Kallmans syndrome also lower testosterone levels.
 ,
"Our bone health is largely dependent on the genes we inherit from our parents."
 ,
• Hyperthyroidism, when levels of thyroid hormone are abnormally high.
• Parathyroid disease, when levels of parathyroid hormone are abnormally high.
• Conditions that affect the absorption of food such as Crohns or coeliac disease.
• Conditions that cause long periods of immobility.
Other conditions may be associated with osteoporosis, such as diabetes and HIV (AIDS). People who have had an organ transplant or who have experienced respiratory diseases may also be at increased risk, as well as people who have undergone gender reassignment especially if hormone therapy is discontinued.
Some medicines increase your risk:
• Taking corticosteroid tablets for other medical conditions for over three months.
• Anti-epileptic drugs.
• Breast cancer treatments such as aromatase inhibitors.
• Prostate cancer drugs that affect either the production of the male hormone testosterone or the way it works in the body.
• Some medicines may increase risk but more research is needed.
• Injectable progestogen contraceptives –medroxyprogesterone acetate (Depo provera).
• Some drugs used for mental health problems (particularly psychosis).
Other risk factors include:
• Smoking – current smokers are more likely to break bones
• Alcohol – intake of more than 3 units daily
• Falling – older people who are at risk of falling are more likely to have fractures especially of the hip after the age of 75 years.
How is osteoporosis diagnosed?
If you are concerned about your bone health you should talk to your GP, who might refer you for a DXA Scan. A Dual energy X-ray Absorptiometry (DXA) scan is the gold standard in diagnosing osteoporosis. It is a simple, painless procedure and is recommended for those considered to be at high risk of breaking a bone due to osteoporosis and who might need a drug treatment to strengthen their bones.
 ,
"...drugs help increase bone density, strengthen bones and lower the risk of fracture by about 50%."
 ,
It’s worth bearing in mind that osteoporosis diagnosed from a bone density scan does not necessarily mean that the patient is at high risk of breaking a bone at that time, so a drug treatment therefore is not always necessary.
What treatments are available?
Treatments for osteoporosis aim to reduce the risk of broken bones occurring and there is a range of drug treatments that have been shown to do this. Most drugs work by slowing down the activity of the osteoclast cells that break down old bone – anti-resorptive drugs. Some treatments stimulate the cells that build new bone – anabolic drugs.
Bisphosphonates are the most commonly prescribed drugs used to treat osteoporosis. These include alendronic acid or alendronate, cyclical etidronate, ibandronate, risedronate and zoledronic acid.
Other drug treatments for osteoporosis include:
• Raloxifene,
• Strontium ranelate,
• Parathyroid hormone (PTH) treatment,
• Denosumab.
Calcium and vitamin D supplements are often prescribed by doctors to older people to help prevent broken bones.
All of these drugs help increase bone density, strengthen bones and lower the risk of fracture by about 50%.
How can I look after my bones?
Most of us take our bones for granted and tend to forget that our bones are a living tissue, but we should look after them throughout our lives in the same way that we look after our heart, lungs and even our hair and skin.
Our bones are at their strongest in our mid-twenties, so it’s crucial to build them up when we are young and then to continue looking after them throughout our lives.
By eating a calcium-rich, healthy balanced diet, getting lots of weight-bearing exercise and maintaining vitamin D levels through safe summer sunlight, we can all keep our bones healthy for longer.
What does the future hold for patients with osteoporosis?
The population of the UK is getting older – by 2034, 23% of the population is projected to be aged 65 and over.
By 2030 in England, the number of hip fractures in men will have surpassed those suffered by women.
By 2036, on current trends, the hospital admissions for hip fractures in men across the UK will almost match those for women and the cost of treating and caring for hip fractures in the UK could top £6billion.
If we do not act now to improve the prevention, diagnosis, treatment and care of osteoporosis, the number of people affected by fractures will rise steeply in just a few years.
 ,
"...act now to improve the prevention, diagnosis, treatment and care of osteoporosis..."
 ,
We must all work together to ensure that people who suffer fragility fractures are identified, assessed and treated in an appropriate and timely manner.
The National Osteoporosis Society is working in collaboration with Age UK to lead the new Falls and Fractures Alliance, which gives responsibility to health professionals, NHS and the Government and which will ensure that the numbers of falls related fractures are cut, saving loves and saving money.
Some previous ‘Spotlight on…’ articles:
About the author:
Siobhan Hallmark has been the Press Officer at the National Osteoporosis Society since 2007, during which time she has worked to ensure the general public, patients and health professionals have a better understanding of importance of healthy bones and of the impact of osteoporosis and fragility fractures.
The National Osteoporosis Society is the only UK-wide charity dedicated to improving the prevention, diagnosis and treatment of osteoporosis and fragility fractures. In the UK, one in two women and one in five men will break a bone, mainly because of poor bone health.
We work to: increase understanding and awareness of osteoporosis, inform and unite health professionals, fund research into osteoporosis and fractures resulting from fragile bones, influence governments and healthcare providers to offer systematic, high-quality care for people at risk of fractures, and offer caring support to those affected by osteoporosis.
We are an independent charity. Our funding base consists of legacies, personal donations, membership fees, fundraising programmes and modest contributions from industry. We do not receive funding from any government or the NHS.
How can pharma improve osteoporosis treatment?