UK’s drug supply contingency plan for hard Brexit
The UK government has issued several documents to help businesses in planning for the eventuality of a no-deal Brexit, but the UK’s Brexit Health Alliance says “the guidance is a first step, but only a first step” as several questions remain unanswered.
The pharmaceutical industry has been voicing its concerns about the possibility of a no-deal Brexit for months, with access to medicines being at the forefront of its concerns.
Pre-Brexit anxiety
Two weeks ago, pharmaphorum reported on an unsettling email from NHS Providers, which was leaked to The Times, about the poor coordination between ministers and the health service.
In this correspondence Chris Hopson, the chief executive of NHS Providers described his concerns about no-deal Brexit and advised it “could disrupt the entire supply chain of pharmaceuticals”.
The Association of the British Pharmaceutical Industry (ABPI) was also concerned that there were no firm arrangements about an implementation period for Brexit, and the role of the UK drugs regulator after the country leaves the EU.
Health secretary’s letters to pharma
In response, the UK health and social care secretary Matt Hancock outlined his contingency plans in two letters: one to pharmaceutical companies, and one to the chain of suppliers of medical devices and clinical consumables.
“The government has made significant progress in negotiations with the EU and remains confident we will leave with a good deal for both sides, that supports existing and future healthcare collaboration,” said Hancock.
“However, as a responsible government, we continue to prepare proportionately for all scenarios, including the unlikely outcome that we leave the EU without any deal in March 2019.”
“Given the significant amount of work that has now been done, I am confident this gives a clear basis for the health and care sector and the life sciences industry to plan so that patients can continue to receive high-quality care unhindered.”
Pharma has pledged to increase their drug stocks by at least six weeks on top of their usual buffer supply, ensuring plans are in place to air freight products with a short shelf life that cannot be stockpiled.
Medical device suppliers have been assured that separate contingency plans are being developed, including increasing the national level of stock holding, and have been asked to hold off for “further information until September”.
Industry already one step ahead of the government
Hancock’s request has been called by Steve Bates, CEO of the UK Bioindustry Association (BIA) as a “massive challenge” for pharmaceutical companies to deliver in less than 200 days.
But the government’s request did not come as a surprise to some of pharma’s giants who were stockpiling drugs well before Matt Hancock’s letters. Sanofi and AstraZeneca were reported to be increasing contingency supplies by four weeks at the beginning of August 2018, fearing border delays and complications in a post-Brexit UK.
Hugo Fry, managing director of Sanofi’s UK operation, said the group had started to plan for additional warehouse capacity to store stocks of its products and “increase UK-based resource to prepare for any changes to customs or regulatory processes.”
Sanofi has also stated that a no-deal Brexit scenario will make its current quality control set-up impossible, as it sends batches of drugs back and forth across the channel.
Hancock’s optimism startles MPs
However, the UK health secretary remains optimistic about contingency plans, advising hospitals, GPs and pharmacies not to hoard or stockpile additional drugs beyond their usual level.
“There is no need for clinicians to write longer NHS prescriptions,” he said. “Local stockpiling is not necessary and any incidences involving over-ordering medicines will be investigated.”
“Clinicians should advise patients that the government has plans in place to ensure a continued supply of medicines to patients from the moment we leave the EU. Patients will not need and should not seek to store additional medicines at home.”
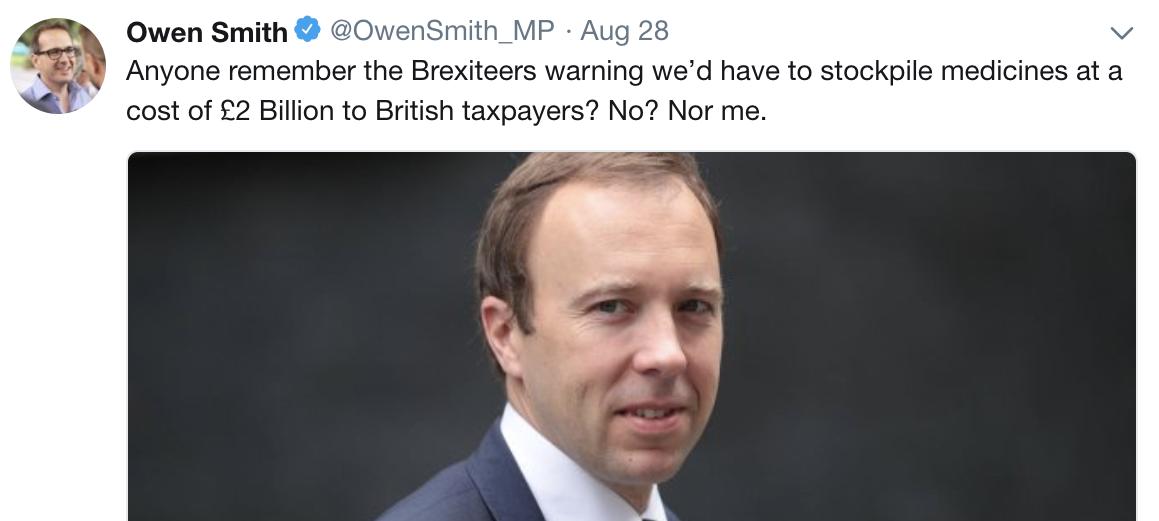
Hancock’s letters and warnings sparked a series of parliamentary comments with the supporter of pro-EU  campaign, Labour MP Owen Smith saying:
campaign, Labour MP Owen Smith saying:
“How on earth have we ended up in a situation where the government needs to ensure Britain is prepared to have medicines flown in, in order to protect the lives of patients?”
“I don’t remember anyone warning that Brexit would mean we’d have to stockpile drugs or that this would cost the NHS and taxpayers up to £2bn. Maybe they should have slapped that on the side of the bus.”
The official technical guidelines
Although the government is insisting it is highly unlikely that Theresa May will not be able to strike a deal with negotiators in Brussels, it has published a series of documents to help businesses plan for a no-deal scenario, including details about regulation of medicines, batch testing, safety and quality of blood and organs as well as clinical trials.
The technical notices give pharmaceutical companies clarity that in the event of a no-deal, the UK government will take a pragmatic approach to the regulation of medicines by recognising and using medicines and vaccines which have been licensed and manufactured in the EU.
Mike Thompson, chief executive of the ABPI, commented on the government guidance: “By agreeing to recognise and use medicines and vaccines licensed and manufactured in the EU, the UK Government has taken an important step to protect patients. We urge the EU Commission to do the same.”
“We need to be clear that a no-deal scenario is not in the interest of patients. Both sides must rapidly agree the terms of the UK’s withdrawal and a future relationship based on cooperation to protect public health, control infectious diseases and manage medicine safety.”
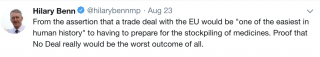 The senior Labour MP Hilary Benn, who chairs parliament’s Brexit Select Committee, said “a lot of questions remain to be answered” following the publication of the documents.
The senior Labour MP Hilary Benn, who chairs parliament’s Brexit Select Committee, said “a lot of questions remain to be answered” following the publication of the documents.
“These papers confirm that no-deal, far from being better than a bad deal, would be very damaging economically.”
“Businesses that export to the EU would face the cost and bureaucracy of customs, safety and security and rules of origin declarations for the first time, and in certain sectors, tariffs.”
“Having wasted two years, these papers show exactly why no-deal is unacceptable and why ministers must now ensure that an agreement is reached with the EU which provides a transition period and protects jobs, trade and investment.”
Pharmaceutical industry cautiously optimistic – but we still need a deal
The UK Bioindustry Association welcomed the government's documents as helpful; however, they look forward “to further discussion of the detail to build greater clarity around how the complex regulation and supply of medicines would work in the event of no-deal.”
“We encourage pharmaceutical companies that supply medicines for NHS patients from, or via, the European Union or EEA, to engage actively with the Department of Health's request for information as to how, or whether, they can, or cannot, ensure an additional minimum of six weeks supply in the UK, over and above their business as usual operational buffer stocks, by 29th March 2019,” said Steve Bates.
The UK’s Healthcare Distribution Association, which represents drug wholesalers, believes that the government approach “is sensible and pragmatic at this stage” but added that a Brexit agreement must still be Theresa May's primary objective in Brussels.
Niall Dickson, co-chair of the Brexit Health Alliance, an umbrella organisation representing stakeholders from the NHS, medical research, industry, patients and public health organisations said: “What we need is a categorical assurance that patients will continue to get the medicines and treatment they need, no matter what happens in the negotiations. This guidance is a first step, but only a first step, towards that.”
What next?
The UK government is currently seeking evidence on contingency plans from pharma. Industry has until 10 September to reply to the health secretary’s letter confirming their plans on a product-by-product basis.
The October EU Council meeting will become increasingly significant and the UK Brexit secretary, Dominic Raab and the EU chief negotiator Michel Barnier have agreed that the negotiations will progress on a weekly basis in the run up to that meeting.
“What is clear is that the UK Government and the EU Commission agree there needs to be a deal”, said Mike Thompson, the ABPI’s CEO directly to Dominic Raab at the press conference after his speech.
“We need the full focus of the Government on getting the right deal”, said Elliot Dunster, head of External Affairs at the ABPI.
Despite difference in opinion, there is one key message to the British government, which everyone is agreed on: getting a deal, which includes cooperation on medicines, is in the best interests for patients not just in the UK but in the EU as well.